Neonatology
A concentration of scientists and clinicians embedded in the Research Department of Neonatology within the EGA Institute for Women’s Health at UCL focuses on innovation in diagnosis and therapy to improve outcomes of babies with common perinatal and neonatal problems. There are particular strengths in acute care of the preterm newborn infant in neonatal respiratory and intensive care and in neonatal neuroscience including developing novel therapy for lung disease and birth asphyxia combined with advanced neuromonitoring via optical and magnetic resonance techniques for biomarker discovery and validation. The Department is a major centre for clinical innovation in neonatology whose investigators have international reputations for pioneering new diagnosis and therapy for brain and lung injury in babies.
Professor Howard Clark leads the Research Department of Neonatology and his group focuses on developing better treatments for Neonatal Respiratory Distress Syndrome (RDS) which aim to reduce the incidence of neonatal chronic lung disease and improve neonatal outcomes after preterm birth by Targeted Lung Immunotherapy.
Professor Nicola Robertson has led the neonatal neuroscience group to major advances in the understanding of therapeutic hypothermia and novel neuroprotective strategies following perinatal hypoxic ischaemia. Her group focuses on translating these laboratory discoveries into novel therapy in the clinical care of the newborn with brain injury.
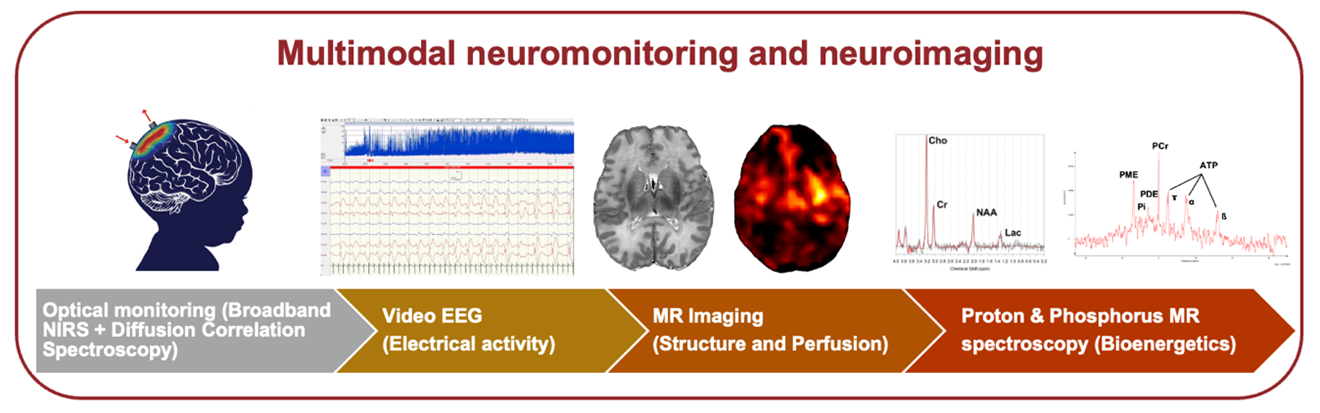
Dr Subhabrata Mitra joined the Institute in 2016 and is leading advances in neuromonitoring and neuroimaging in neonatal seizures and neonatal encephalopathy. The group’s research focusses on optimising brain monitoring for better understanding of pathophysiological changes and development of early biomarkers following perinatal brain injury. The group is also developing a non-invasive optical tool to assess placental function that will result in a better understanding of the physiological changes related to preterm delivery and stillbirth.
Professor Neil Marlow's work on preterm brain injury and developmental outcomes made UCL a leading centre for work on longitudinal cohort studies, such as EPICure, pioneering the investigation of the preterm brain combining imaging and novel neuropsychological strategies.
Research groups
Research focuses on developing new therapeutic intervention for neonatal lung disease based on his internationally recognised expertise in lung surfactant proteins. This work has been recognised by substantial awards from the Medical Research Council to carry out first in man trials of novel surfactant protein immunotherapy.

The group focuses on the development and optimisation of a non-invasive optical monitoring tool for a better understanding of fetoplacental function to improve perinatal outcomes, with particular interest in the prevention of stillbirth (PROPEKT study funded by Wellcome Leap) and identifying mechanisms related to preterm birth (PreNIRS study funded Tommy’s Charity and Wellcome / EPSRC Centre for Interventional and Surgical Sciences (WEISS)).

The group is investigating the impact of seizures on the newborn brain in a Wellcome Trust funded study, working in collaboration with the Biomedical Optics Research Laboratory (BORL) at UCL and the Infant Research Centre at University College Cork. The project includes a preclinical component (in collaboration with the Preclinical Neonatal Neuroprotection group at UCL) and a clinical study at UCLH.
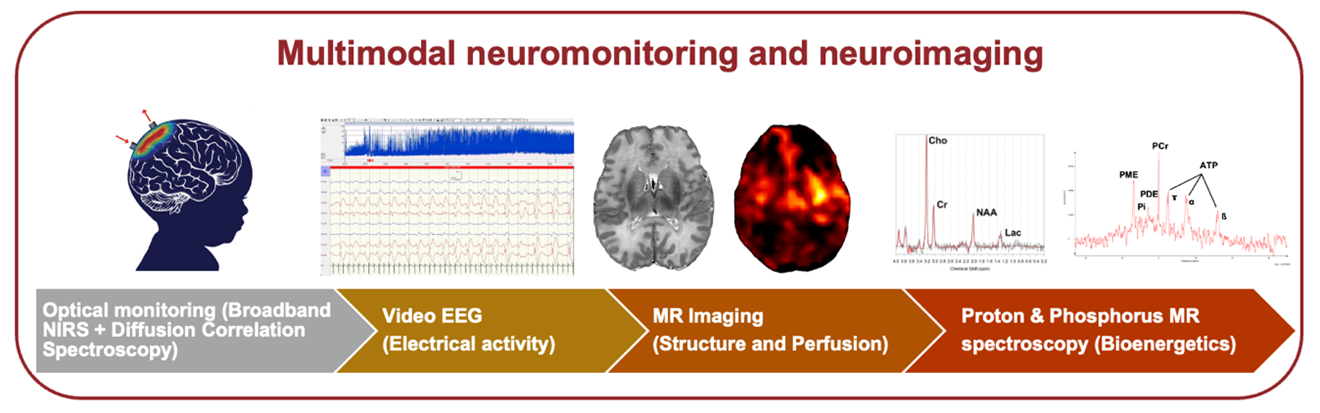
We use a multimodal platform of advanced optical neuromonitoring, systemic physiological data, neurophysiology (video EEG), magnetic resonance imaging and spectroscopy (MRI and MRS) to develop early biomarkers of perinatal brain injury for accurate assessment of injury severity and outcome prediction.

UCH Neonatal Services contributes to clinical trials and studies, which are mulicentre - recent studies have included the HTA funded PIPS and two UCL-based FP7 funded studies: NEMO and EVERREST. New studies are currently under consideration.

Long term outcomes for babies born very prematurely or following perinatal asphyxia are improving. We are investigating these long-term effects from epidemiological and neuroscience perspectives grounded on national and local cohort studies.

Our aim is to optimize and refine neuroprotection of the term infant using a translational pre-clinical model of perinatal asphyxia. Our team includes neonatologists, physicists and scientists. We are focus on magnetic resonance, EEG and NIRS biomakers which can be used interchangeably in clinical studies.

Globally, newborn brain injury is the third leading cause of childhood mortality. With partners in Uganda, the UK and Australia we are investigating the aetiology of, and outcomes from newborn brain injury to help prevent future newborn detahs and long-term disability.

We are a unique team of neonatologists, neuroscientists, clinical neurophysiologists and statistical scientists who are working together to discover how newborn infants process touch, pressure and pain.

Understanding the molecular signals triggered in the developing brain and designing therapies to optimise neurological outcomes following preterm birth and labour complications.

We are a unique team of neonatal nurses investigating ways to improve patient care and parent experience.

Explore the lists of research students within our Research Department of Neonatology and visit their profiles.
 Close
Close