Adult vitelliform Macular Degeneration (AVMD) is an adult onset form of Bests disease.
What is Adult vitelliform Macular Degeneration (AVMD)?
AVMD is a dominantly inherited bestrophinopathy which affects the Retinal Pigment Epithelium (RPE). It is very similar to Best disease (learn more Best disease here), so much so that many argue that AVMD is a form of Best disease. The number of patients suffering from AVMD is not currently known, though, it is a rarer incidence than Best disease. Typical age of onset of the condition is between 30 to 50 years old. AVMD has also been found to be caused by mutations in the PRPH2 gene, as well as the BEST1 gene.
How does AVMD affect the eye?
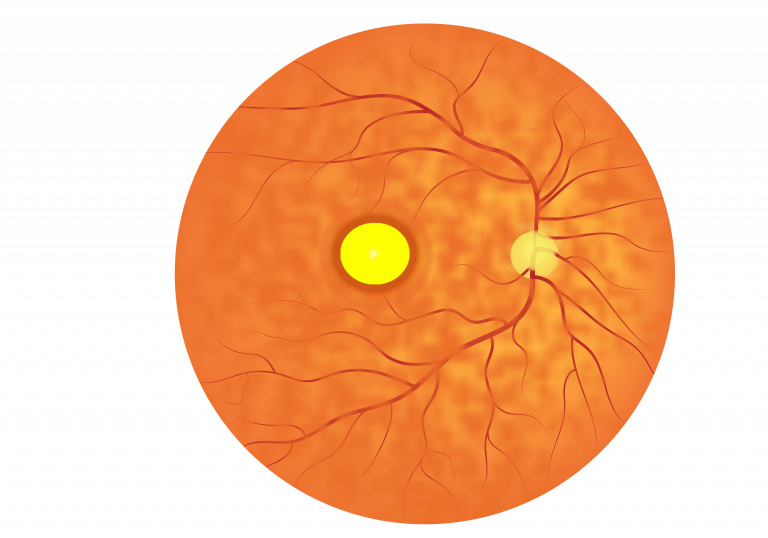
AVMD is clinically indistinguishable from milder forms of Best disease, with the classical vitelliform ‘egg-yolk’ lesion also usually being present. AVMD has even been said to be a less severe form of Bests, owing to the fact that it begins later than Bests and also seems to have a much slower progression. The ‘egg-yolk’ lesions also appear to be much smaller. These smaller lesions may not necessarily pass through the six clinical stages of Best disease but the region may still undergo atrophy (death of the region).
AVMD has a less dramatic effect on vision, compared to Best disease. In general, older patients are diagnosed when changes in their macular region are observed, these changes may or may not be accompanied by vision loss. Over time, central vision loss can occur, but vision tends to remain stable, however AVMD patients can have complications associated with the disease. Vision has been reported to range from 6/12 to 6/60 on the Snellen chart.
How is AVMD diagnosed?
Similar to Best disease, OCT imagery can be used to examine the macular region, assessing any lesions, RPE structure, lipofuscin deposits and fluid build-up.
Autofluorescence imaging (FAF and FA) can be used to detect the hyperautofluroscence seen at earlier stages, and hypofluorescence at late stage disease. EOG recordings, however, are usually normal or only slightly reduced in AVMD patients. ERG recordings will also be normal in those suffering with AVMD.
Suspected cases of AVMD can be confirmed using genetic sequencing.
Are there any complications associated with AVMD?
The main complication for AVMD is choroidal neovascularization (CNV). This is where new and weak blood vessels, which originate from the choroid, make their way through the RPE layer of cells. The new blood vessels can easily rupture and break leading to fluid leakage. The build up of fluid can lead to pigment epithelial detachment (PED). PED is another complication of AVMD and it occurs when excess fluid build-up causes the RPE to detach from the underlying choroid.
What are the treatment options for AVMD?
There are currently no medical or surgical treatment options available for AVMD, or any of the bestrophinopathies, however research is ongoing and promising. The complications associated with AVMD can be treated, e.g. anti-VEGF injections used to stop the growth of newer vessels, with the aim to preserve vision.
Research into treatments for AVMD is ongoing. Patients are encouraged to visit the many charities and support groups for bestrophinopathies.
 Close
Close

