Spotlight on ECRs: Dr. Nish Arulkumaran
Dr. Nishkantha (Nish) Arulkumaran shares his recent publication success and career journey as a clinical scientist in research.

12 November 2023
Interview by Dr Zoe Whiteman & Dr Marie-Belle El Mdawar, UCL Respiratory
Nish is an honorary associate professor at UCL Department of Medicine and a consultant in intensive care medicine at UCL Hospital, where he started working in February 2020.
When he started his postgraduate training as a doctor, he knew that he wanted to become an intensive care physician but at that time, intensive care medicine was a postgraduate specialty. He enjoyed the nephrology as a junior doctor, so he decided to specialise in nephrology and subsequently in intensive care medicine. It was useful because there is important overlap between the two specialties. Additionally, nephrology involves a lot of pathology and immunology, which is relevant for his current research.
However, he currently doesn’t practise as a nephrologist simply because there aren't enough hours in the day.
Research Questions
Thanks very much for joining us today, Nish.
1. We will start at the beginning of your career journey. As a clinical scientist, what motivated you to pursue a career in research and how do you combine your MD and PhD titles?
Nish: As a clinician, my approach to research pivots on clinical problems that I encounter. A career in translational medicine provides the opportunity to develop ways to improve the health of patients. Working in intensive care, I often looked after patients with life threatening infections who require organ support. In the recent decades, antibiotic resistance has become a global threat. After the discovery of penicillin almost a century ago, we have been through the Golden age of antibiotics with patients benefiting from this. Several medical procedures would have otherwise been impossible. The lack of effective antibiotics, which might be a reality in the future, means that straightforward procedures including some routine surgery will become increasingly dangerous. Also, there haven't been any new classes of antibiotics in clinical practice since the 1990’s. My research focuses on the use of liposomes and nanoparticles to improve the efficacy of the existing antibiotics. That is how my clinical work and lab work are linked.
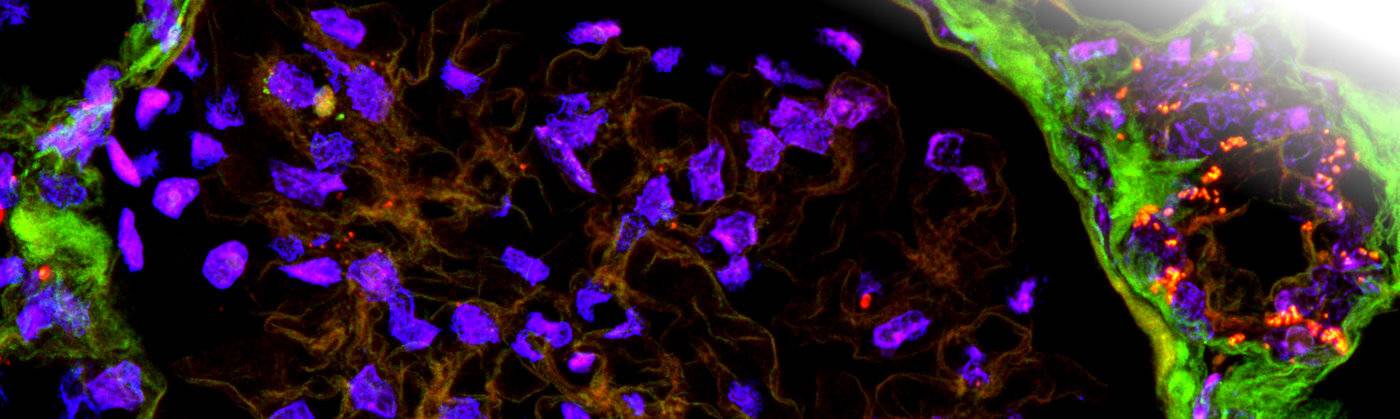
2. You recently published an interesting article in Nature communication about “Creating complex protocells and prototissues using simple DNA building blocks”. Can you briefly summarize this study and its impact on medicine?
Nish: We are currently exploring the possibility of using nucleotides as a therapeutic strategy to fight pathogenic bacteria. Two of the co-authors, John Burns and Stefan Howorka, are both chemists who specialise in DNA nanotechnology. We are looking to see whether we can harness the use of DNA or nucleotides to fight antimicrobial resistance; one potential way is to create a synthetic neutrophil extracellular trap to capture bacteria, and another potential way is to use a nucleotide strand as an antisense oligonucleotide to inhibit translation of bacterial mRNA for resistance proteins. Either way, the nucleotide is packaged within liposomes as delivery vehicles in a very similar fashion to the mRNA COVID vaccine. The manuscript that we published describes the principles and versatility of incorporating nucleotides within liposomes, which underpins our ongoing work.
3. What is your current focus in research? And are there any students working with you? If yes, how would you describe the relationship you have with them?
Nish: The aim is to create a safe and cost-effective way to improve on existing antibiotics and to overcome antimicrobial resistance. This work is being done in collaboration with UCL chemistry, specifically with Prof. Stefan Howorka and his post-doc Dr. Jon Burns. In parallel, I am investigating the potentially deleterious effects of antibiotics on the host immune system. Better knowledge on this might improve antibiotic stewardship.
We have a couple of PhD students in the lab, as well as a couple of BSc students. One of the PhD students is an intensive care clinician who spending half his time in clinical work and the other half doing a part-time PhD. The other PhD student is a medical doctor from Pakistan. The two BSc students are here over a period of six months to do laboratory work and they are helping with ongoing projects. The four students who are part of the team integrate well with each other but also have very independent aspects to their projects so that they can take some ownership and develop their own interests. They work together and count on each other for practical assistance, moral support, and ultimately publishing work together.
4. You are also interested in systematic reviews and Meta-analysis with 2 published recently on the “Association Between Hypocholesterolemia and Mortality in Critically Ill Patients With Sepsis” and “Effect of Corticosteroids on Mortality and Clinical Cure in Community-Acquired Pneumonia”. What drives you to participate or initiate such studies and how much of your clinical and/or scientist backgrounds are involved in putting in place such investigations?
Nish: The need to do systematic reviews, from my perspective, stems from the need to understand the literature before you embark on your own research. It is important to know what has already been done before doing your own research; and a way to get an objective idea about the work that is being done is to conduct a formal search across different databases and amalgamate all the literature in a structured way. This allows one to understand in an objective and clear way the work that has already been performed, to inform your own research.
As a clinician, the other reason why I am interested in systematic reviews and meta-analysis is to evaluate clinical trials and studies. This was particularly important during Covid; there were several clinical trials being conducted of different interventions ranging from IL-6 receptor antibodies to steroids. One way to amalgamate and understand all that information, is to conduct a formal review of the literature and get a very objective, clear view on what the intervention is and to which patient population it is applicable to, but also what clinically relevant outcomes one might achieve from that intervention.
5. Can you tell us something amazing about the kidney that people may not know?
Nish: One interesting concept or paradigm is about what clinicians or doctors call acute renal failure. When a patient is unwell and they stop passing urine with an increase in the kidney biomarker (creatinine), we call it acute renal failure. But if we really think about it, that is a normal physiological response: it is normal for the body to stop passing urine and as a consequence the biomarkers go up, which is a protective mechanism. So I don't always like to use the word “renal failure”, but rather I sometimes wonder whether we fail to understand the kidney.
6. Can you tell us about a setback that you might have encountered and how you were able to overcome it?
Nish: I suppose, like all researchers, the need to secure grant funding is probably one of the most challenging issues. I was recently invited for a fellowship interview at the Wellcome Trust, and I was unsuccessful. The standard was high, as reflected by the feedback. However, the feedback from the rejection gave me some tangible goals to try and achieve over the next year, and it also made me focus more on what was achievable and what was important. There were some very positive points as well, which has provided me with some motivation and encouragement to try and improve.
7. Would you like to share something interesting that you have read about recently?
Nish: One of the recent papers I read was about the use of monoclonal antibodies to target tissues more selectively. A lot of research has been devoted towards optimising monoclonal antibody efficacy and safety; one strategy that has gained attention recently uses 2 targets in proximity on the cell surface receptor to trigger a response, and this concept has already been achieved using CAR-T cells with synthetic signaling pathways. The investigators who published in Nature Biotech (Oostindie S, et al. Nat Biotech, 2022) use monoclonal antibody constructs designed to oligomerize and trigger complement-dependent cytotoxicity on cells that express 2 specific antigens. This technology, which they call HexElect, involves the introduction of complementary mutations on the Fc-Fc monoclonal antibody interface with the aim of enhancing efficacy, whilst limiting cytotoxicity to cells expressing only one antigen. As a clinician scientist, I would hope that one can significantly enhance selectivity of monoclonal antibody treatment to the target tissue whilst simultaneously limiting the off-target effects.
Personal / Opinion questions
1. Reflecting on your research journey so far, what are you most proud of attaining or achieving?
Nish: Looking back, there is not any specific piece of work that I would highlight. However, my work during the COVID-19 pandemic was challenging. I led some observational, clinical and translational studies in addition to collaborating on interventional studies. In addition, we provided timely meta- analyses on multiple clinical trials pertaining to COVID-19 treatments, which guided clinical care. I was a newly appointed consultant in intensive care medicine at the time, and the workload was intense. But despite that, as a team, we managed to deliver some clinically relevant research.
2. As a clinical scientist, how did you find the transition to learn lab-based skills and which one you enjoy the most?
Nish: As a clinician, I haven't got the same background as a scientist, so I am dependent on my scientist colleagues for their knowledge and skills. During my PhD I took on a translational project looking at the use of a novel drug to prevent acute renal failure in an animal model of sepsis. I acquired relevant skills both from existing PhD students and postdoctoral scientists in the lab.
A skill that I find most rewarding and challenging is creating a clinically relevant animal model of disease. There are a lot of constraints when it comes to animal models, including some different biological responses across species, and the limitations in medical interventions. As an intensive care physician, a relevant model for me would involve providing multiple organ support to manage critical illness over a number of days which is clearly not practical in an animal model. Trying to overcome such limitations is very challenging but rewarding.
3. Do you have any advice for PhD students and/or early career researchers who are starting their PhD/research journey?
Nish: It is important to seek a nurturing environment and mentor. A mentor doesn't have to be your PhD supervisor, and sometimes it might be helpful to get a mentor who isn't; so to get an objective point of view. And a mentor can either be a PostDoc or even a more senior PhD fellow within the same lab, or a different lab.
4. Outside research and clinical duties, what interests and activities do you like to pursue?
Nish: At the minute, the thing that keeps me most busy is family. I've got two boys, aged five and eight, and my wife is also an academic clinician; trying to balance both careers and family life is challenging. Before the COVID pandemic, my wife and I enjoyed travelling a lot and now that the pandemic has subsided we're excited to continue that again.
5. People are more aware now about their mental health and are trying to have a more balanced work/life load. How do you manage yours? and is there any tips you would like to share with ECRs that you find beneficial to your mental health, inside and outside the lab?
Nish: I'll be honest- I probably haven't worked it out yet. I think we've all got different responsibilities. For instance, I have my clinical commitments, my academic commitments, teaching commitments, and family commitments which I have to fit into a 24- hour day. Priorities change over time and one needs to learn how to adapt.
I've learned to accept that I only have 24 hours in a day and only so much can be achieved. This is not unique to myself. I think a lot of us clearly are ambitious, which is great. However, I think sometimes taking a step back and accepting that given the current circumstances, what we're achieving is commendable.
6. Do you have a favourite quotation or an inspiring memo that you would like to share with our readers?
Nish: One interesting quote is from Edwin Hubble, who said that ‘equipped with these five Senses, Man explores the universe around him and calls this adventure science.’
As a clinician scientist that's quite relevant; to understand and explore what I see and experience clinically, within the lab.
 Close
Close

