Full Results from Huntingtin Lowering Antisense Oligonucleotides Trial now published
7 May 2019
The first drug targeting the cause of Huntington’s disease was safe and well tolerated in its first human trial, and successfully lowered the level of the harmful huntingtin protein in the nervous system.
After over a decade of pre-clinical development, this human trial of huntingtin-lowering drug began in August 2015 and completed in late 2017 and was the first study to show antisense oligonucleotide (ASO) mediated suppression of a toxic protein in the brains of adults with this neurodegenerative disease. The trial, led by Professor Sarah Tabrizi (Director UCL HD Centre, UCL Queen Square Institute of Neurology, and UK DRI at UCL) and sponsored by Ionis Pharmaceuticals, involved 46 patients with early Huntington’s disease at nine study centres in UK, Germany and Canada. The top-level trial results were announced in December 2017 and now the full set of results, including the decade of pre-clinical modelling work, have been published in the prestigious New England Journal of Medicine.
Huntington’s disease is an autosomal dominant neurodegenerative disease caused by a CAG repeat expansion in the huntingtin gene (HTT) resulting in the production of toxic mutant huntingtin protein (mHTT). The drug trialled IONIS-HTTRx (now RG6042), is an ASO discovered and developed by Ionis to inhibit the huntingtin messenger RNA and thereby reduce the levels of mHTT. The trial was a randomised, double-blind, multiple ascending dose, Phase 1/2a study in adults with early Huntington’s disease. Participants received the drug or placebo (3:1) via bolus intrathecal administration every four weeks for four doses. Dose selection was guided by a pre-clinical model relating dose levels to reduction in huntingtin. The primary endpoint of the trial was safety. Pre-specified exploratory endpoints included the concentration of mHTT in cerebrospinal fluid (CSF).
Of 46 patients involved in the study, 34 were randomised to receive the drug at doses of 10-120 mg, and 12 were randomised to receive placebo. Each participant received all four doses and completed the study. No serious adverse events were recorded in patients who received the drug, and there were no clinically relevant adverse laboratory or parameter changes. The drug treatment resulted in dose dependant reduction in CSF mHTT with a mean lowering of 40% for the higher dose groups, with some patients reaching 60% lowering.
Professor Sarah Tabrizi, lead author of the New England Journal of Medicine manuscript, said: "I am so pleased now that the full trial results including critical pre-clinical model are now published in the New England Journal of Medicine. We are excited to be moving forward to a global Phase 3 trial sponsored by F. Hoffmann-La Roche, which licensed the medicine, to see if regular intrathecal antisense treatment slows clinical progression of the disease. This is an important time in clinical research for patients and families in Huntington’s disease and we are working together with the global community to help enable this trial.’’
"Peer-reviewed publication of these exciting results from the first successful huntingtin-lowering trial is a crucial step that lets us update and call upon the combined expertise of the global community of HD researchers’’ says Dr Ed Wild, Associate Director, UCL Huntington’s disease centre and co-author on the manuscript.
Professor Michael Hanna (Director of the UCL Queen Square Institute of Neurology) said: "this pioneering trial is of ground-breaking importance to neurodegenerative research and I am proud that it was led from the UCL Queen Square Institute of Neurology, the UCLH National Hospital for Neurology and Neurosurgery and the Leonard Wolfson Experimental Neurology Centre. Huntington’s disease is a devastating disease, and therapeutics that target the genetic cause of the disease are those most likely to make a difference. Importantly, the publication of these results has relevance for ongoing clinical research of ASO-mediated toxic protein reduction in other neurodegenerative diseases, including Alzheimer’s, Parkinson’s and Motor neuron disease.”
Links
- Professor Sarah Tabrizi’s IRIS profile
- Dr Ed Wild’s IRIS profile
- Ionis-HTTRx UCL Press release (Dec 2017)
- Tabrizi et al. Targeting Huntingtin Expression in Patients with Huntington’s Disease. New England Journal of Medicine. Available online May 6, 2019. DOI: 10.1056/NEJMoa1900907
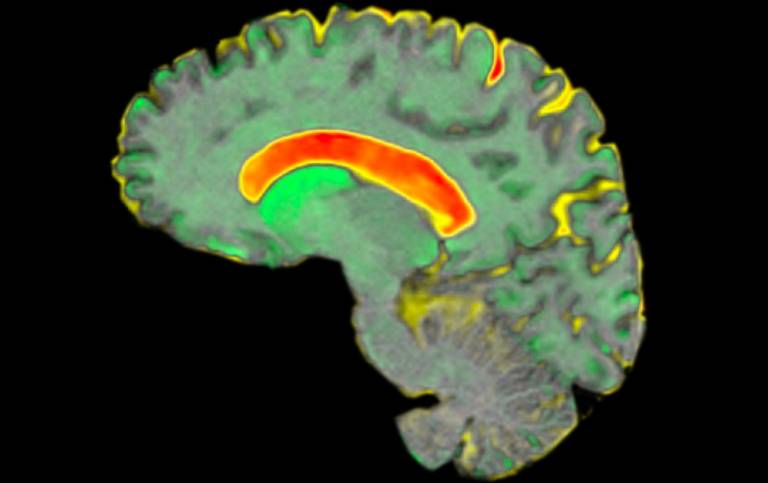
Image
- Regional brain atrophy in Huntington’s disease
- Credit: Dr Rachael Scahill / Track-HD study
 Close
Close

