Public needs to understand who is most vulnerable to COVID-19
23 March 2020
New results on excess 1 year mortality
A new study led by IHI researchers Dr Ami Banerjee, Dr Spiros Denaxas and Dr Laura Pasea along with researchers and clinicians at UCLH, the University of Cambridge and Health Data Research (HDR) UK present new estimates of excess mortality from COVID-19 among those with underlying conditions. Study findings suggest that people with multiple underlying diseases are extremely vulnerable and stronger suppression measures are needed.
The team analysed data from 3.8 million adults in England using UK primary care electronic health records to estimate the excess number of deaths over 1 year under different COVID-19 incidence rates and differing mortality impacts in relation to underlying medical conditions and age. The data show that the UK government’s strategy could lead to between 35,000 and 70,000 excess deaths over the next year, and measures do not go far enough in stopping the spread of the disease or identifying the most high-risk groups. Stronger suppression measures, which aim to reverse epidemic growth, may be required in the UK to avoid excess mortality from coronavirus (COVID-19).
To date nearly all deaths related to the COVID-19 pandemic have occurred in people with underlying health conditions or at older ages, although clinical experience over the last few days suggests that may be changing. Therefore, people with chronic diseases such as heart disease, kidney disease and diabetes, and all older adults are being told to isolate themselves during the COVID-19 outbreak.
However, current models to predict deaths from COVID-19 have ignored underlying conditions or the underlying risk of death, which means that they may not be accurately predicting the number of deaths, and they do not look at excess deaths over a 1-year time frame. The COVID-19 pandemic may cause excess mortality in the population both because of deaths among those infected, and because people who are not infected are experiencing social and economic upheaval; meanwhile the ability of health services to provide high quality of care for both infected and uninfected patients is threatened. This net effect of mortality on the population is thus not only a matter of modelling an infectious disease but modelling a wider societal impact.
The research team used previously validated open-source phenotypes (available at: https://caliberresearch.org/portal), for each condition using ICD-10 diagnosis, Read, procedure and medication codes, and UK Public Health England COVID-19 guidelines (16 March 2020) in 3,862,012 individuals aged ≥30 years from 1997-2017 to report the prevalence of underlying conditions. 1-year mortality was estimated in each condition (and simple models of excess COVID-19-related deaths were developed.
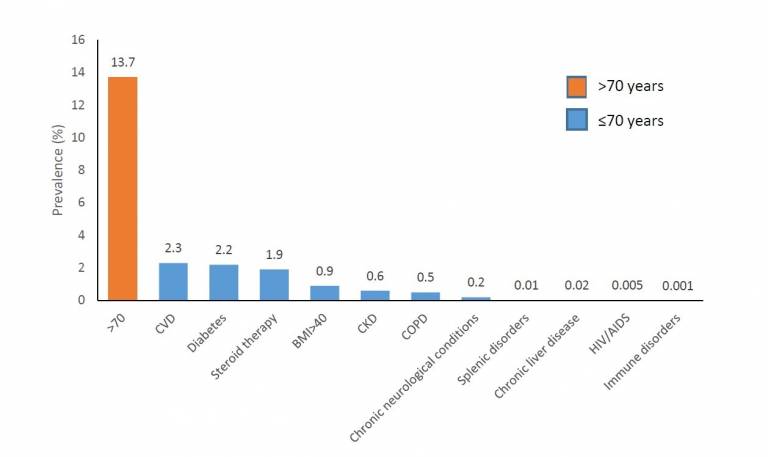
Findings showed that at least 20% of the UK has one of the high-risk underlying conditions for COVID-19 infection, of which, 13.7% were age>70 years and 6.3% aged ≤70 years with ≥1 underlying condition (cardiovascular disease (CVD) (2.3%), diabetes (2.2%), steroid therapy (1.9%), severe obesity (0.9%), chronic kidney disease (CKD)(0.6%) and chronic obstructive pulmonary disease (COPD) (0.5%)). Multimorbidity (co-occurrence of ≥2 conditions in an individual) was common (10.1%).
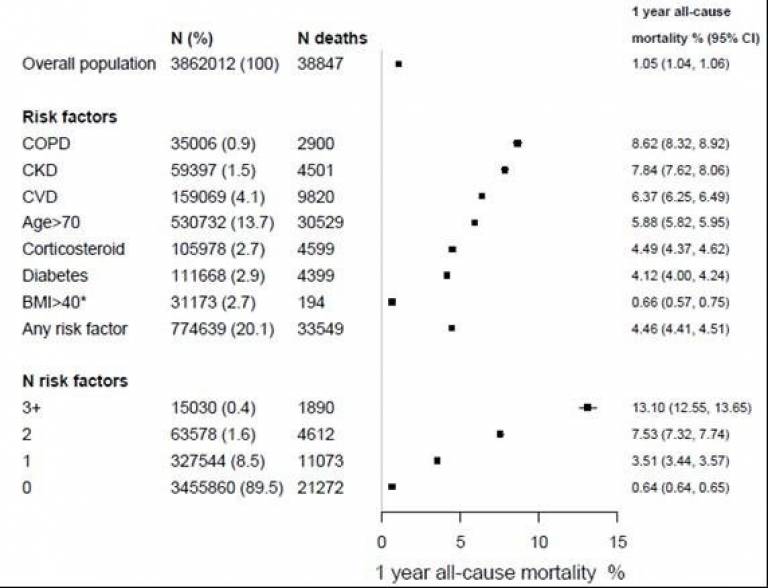
Mortality at 1-year was 4.46% among those aged >70 years or with one or more risk condition. Mortality was 6.4% (95% CI 6.2-6.5%) for CVD, 4.1% (4.0%-4.2%) for diabetes, 7.8% (7.6%-8.1%) for CKD and 8.6% (8.3-8.9%) for COPD. Among those >70 years, one-year mortality rates for COPD, CKD, CVD and diabetes were 13.6(12.9-14.3%), 11.5%(11.0-12.1%), 10.4%(10.1-10.7%) and 8.9%(8.5-9.4%) in men and 12.3%(11.6-13.0%), 9.6%(9.3-10.0%), 10.6%(10.3-10.9%) and 9.8%(9.4-10.2%) in women.
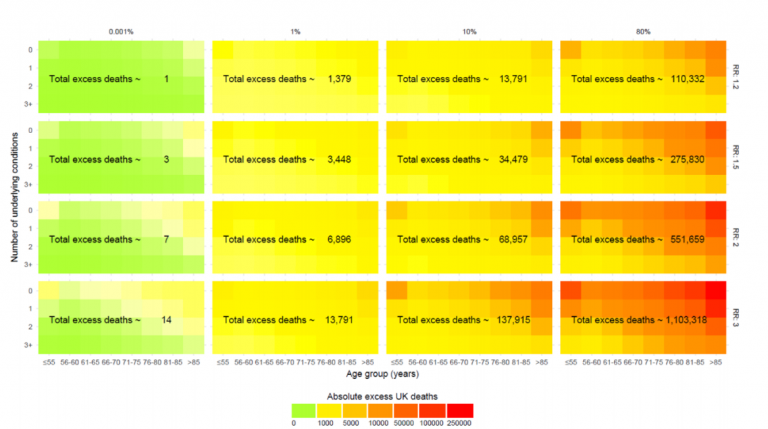
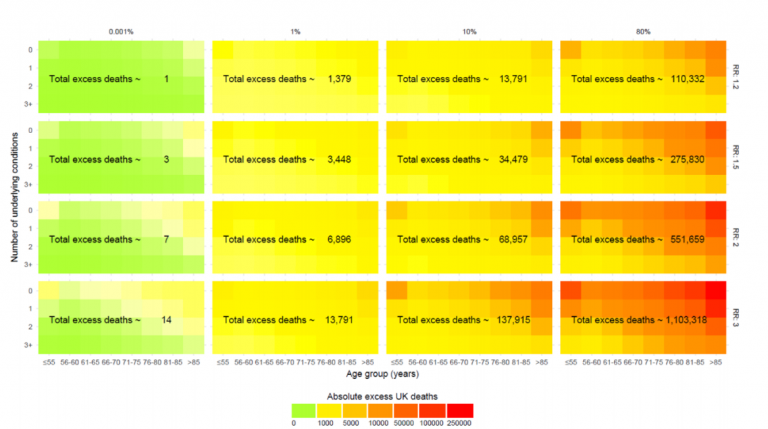
At COVID-19 prevalence of 10% of the UK population (mitigation) and 80% (“do-nothing”), the model estimates 13791 and 110332 excess deaths at RR 1.2; 34479 and 275830 at RR 1.50 and 68957 and 551659 at RR 2.0 respectively. The corresponding deaths at “full suppression” and partial suppression rates of 0.001% and 1% respectively were 1 and 1379, 3 and 3448, and 7 and 6896.
Current targeting of 1.5 million people (about 2.7% of the English population) announced by the Government today may mean that other ‘high risk’ people are not being tested. Lead author, Dr Amitava Banerjee (Associate Professor in Clinical Data Science and Honorary Consultant Cardiologist, UCL Institute of Health Informatics), said: “The UK government is currently following a partial suppression policy of population-wide social distancing, combined with home isolation of cases, as well as school and university closures, but this is currently not mandated. Our study indicates that the government should implement more stringent suppression at population level to avoid not just immediate deaths but also long-term excess deaths.”
The authors conclude that if the relative impact of COVID-19 on mortality over 1 year were 20% (ie. same magnitude as the winter vs summer mortality excess) then the number of excess deaths would be 0 when 1 in 100 000, 14861 when 1 in 10 and 118885 when 8 in 10 are infected. However, if the relative impact is double the mortality risk, then there would be 7, 68957 and 551659 deaths at corresponding levels of infection. These results may inform targeting those at highest risk for a range of preventive interventions.
Based on their analyses, the research team propose three urgent actions:
1. Stringent suppression. The previous mitigation strategy aiming to slow COVID-19 spread could lead to at least 35,000-70,000 excess deaths over 1 year and partial suppression at rising infection rates is inadequate.
2. Public transparency about high risk conditions. The targeting of high-risk 1.5 million people (about 2.7% of the English population) announced yesterday, may miss people at high risk. At least 20% of the UK population has 1 or more high-risk conditions for COVID-19 infection.
3. Massive mobilization of NHS data to drive care, science and innovation to avoid excess COVID-19 deaths. Our study includes only 5% of the UK population's primary care data and what we have is retrospective. Real-time detailed hospital data re. COVID-19 epidemic, e.g. ITU, is not available. This is an unacceptable situation and stops researchers being able to do all the urgent analyses we need to do to tackle this pandemic.
The pre-print paper is available here: https://bit.ly/3aeGlFl
The study is also reported in the press:
Financial Times https://www.ft.com/content/b887d344-6c8b-11ea-89df-41bea055720b.
Daily Mirror https://www.mirror.co.uk/news/politics/coronavirus-government-strategy-could-cause-21737240
Further information on CALIBER is available on the CALIBER website: https://www.ucl.ac.uk/health-informatics/caliber
 Close
Close

