Overview: Pre-term prelabour rupture of the fetal membrane (PPROM) is a major cause of preterm birth. It accounts for 40 % of early infant death and costs the NHS £3 billion annually. Infection, blood and uterine stretch weaken the membrane. Little is known about the factors which initiate the damaging process. PPROM occurs commonly after prenatal fetoscopic and open fetal surgery for identical twin problems and fetal abnormalities. Spontaneous wound healing of the amniotic membrane (AM) does not occur after invasive fetal therapy. A visible membrane defect is seen in the majority of cases. Attempts to seal the defect with glues or decellularised collagen plugs are not clinically effective. Fetal therapy is therefore limited by the complications of prematurity.
Design: We are examining the role of the stretch-sensitive protein connexin-43 (Cx43) in fetal membrane healing and tissue strength. We are also studying the effect of cyclic tensile strain on Cx43 expression and production of inflammatory mediators. With the help of material scientists our aim is to develop a novel bioactive sealing method to heal fetal membrane defects after fetal surgery.
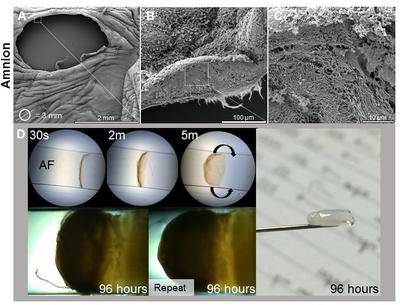
(A-C) Microstructure analysis for the human amniotic membrane following fetoscopy surgery the defect and fibrous architecture of the exposed fetal membrane. (D) Development of novel sealing strategy based on self-assembling membranes at the amniotic fluid interface.
Team: David Barrett (PhD student), Dr Anna David, Dr Chris Thrasivoulou (UCL), Professor David Becker (UCL), Dr. Tina Chowdhury and Dr. Alvaro Mata (Queen Mary University of London), Prof. Jan Deprest and Dr. Alexander Engels (University of Leuven, Belgium), Prof. Che Connon (University of Newcastle).
Funding: Rosetrees Trust, Queen Mary University of London, Prenatal Therapy Charity
 Close
Close







