A hybrid teaching approach transforms the functional anatomy module
An undergraduate module with poor student satisfaction has been turned around by a novel hybrid teaching method, says Dr Nephtali Marina-Gonzalez.
26 September 2018
Academic performance and student experience in a first year module was improved by combining a number of teaching approaches. The success of the approach means it will now be incorporated into the entire curriculum of Applied Medical Science.
Dr Marina-Gonzalez is module lead of Functional Anatomy and Medical Imaging, a first-year module of the Applied Medical Science degree at UCL. In 2017-18 he was also Connected Curriculum fellow in the Arena Centre.
Here, he explains how he successfully combined:
- flipped classroom; where students engaged with the learning material before class, and classroom time was used to deepen their understanding.
- paired discussion; where students shared their reactions to and analysis of learning material with their classmates.
- case-based learning; where students applied their knowledge to real clinical cases.
- freely-available computer-based learning solutions.
His data show that this hybrid learning model, combined with an innovative assessment method, greatly enhanced students’ learning experience and improved academic performance.
The challenges involved in using cadavers to teach
Anatomy has traditionally been considered one of the most fundamental components of medical/biomedical education. Lecture-based teaching supplemented with cadaveric dissection has been the preferred method of teaching since the 16th century.
Although dissection of human cadavers undoubtedly facilitates active learning of anatomy, this practise has many disadvantages, such as:
- emotional stress caused to students
- health and safety-related issues
- significant legal requirements
- exorbitant costs.
Over the last 20 years, initiatives have sought to overcome these problems, in some cases replacing completely the use of human cadavers through the use of:
- prosections (where students learn by either observing a dissection being performed by an experienced anatomist or examining a specimen that has already been dissected by an experienced anatomist)
- plastinated anatomical models
- modern computer based-learning resources
- medical imaging.
These methods require sophisticated equipment, dedicated anatomical models, software licenses and construction of dedicated learning environments. With significant budget constraints and ever-increasing student numbers, these solutions are no longer cost-effective.
Functional Anatomy and Medical Imaging is a very short module (four weeks) which must provide a general overview of human anatomy with a focus on functional aspects, while avoiding unnecessary memorization of facts and hundreds of anatomical terms that would soon be forgotten.
The creation of a hybrid model: what is included?
Having spent years of testing and trying out different teaching approaches in isolation, I decided to create a new hybrid model exploiting the advantages of each method and minimizing their disadvantages.
The resulting hybrid approach has various elements:
Flipped classroom
Online lectures are provided to students (with a duration of ~25 minutes) which they have to watch the day before the face-to-face session.
In addition, students are advised to read selected chapters from an online Anatomy encyclopedia which contains succinct and condensed information in an easy-to-read format and with clinical relevance.
Computer-based learning
Students are introduced to the principles of anatomical structure identification in medical images through online learning.
Using their own laptops and mobile phones, they access an interactive, freely-available picture archiving and communication system (PACS) for in-vivo visualization and assisted identification of normal anatomical structures in X-rays, computer tomography scans and magnetic resonance imaging scans.
In parallel, students are given access to an interactive 3D visualization web-based program to help them identify and correlate the structures visualized in the medical scans with the 3D anatomical illustrations.
Students are allowed to interact with selected images for around five minutes before the presentation of a clinical case. In some other sessions, students are allowed to perform realistic interventional techniques on virtual patients (bronchoscopy and endoscopy) using freely-available mobile simulators for medical professionals.
Case-based learning
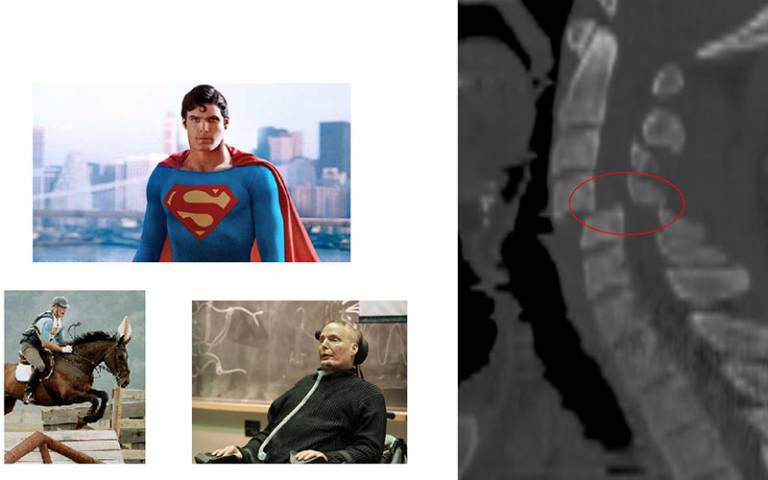
To help students gain insight into pathophysiological processes, they were presented with a real case study which contained interesting and challenging cases with clinical features and laboratory tests.
Paired discussion
A radiological image related to the clinical case is shown without any labels and the students are given the opportunity to spend around two minutes to compare, in silence, the differences between the pathological image with the “normal” image viewed in their PACS system. Students are then asked to discuss the pathological features with their neighbour.
In some instances, students are also instructed to examine each other’s organs where appropriate (e.g. cranial nerves).
Motivational strategy
Students who can describe correctly, and in detail, the pathological image using the appropriate anatomical nomenclature in their final exam presentation are rewarded with an extra point.
Novel assessment
Students create a presentation of a novel imaging technique with special emphasis on its applicability for the study of human anatomy.
This is then presented during a special exam session in front of two examiners and all the students.
- Read the related case study: Novel assessment on anatomy module inspires reconfiguration of assessment on entire programme
Impact of the hybrid teaching model on exam scores and student satisfaction
We compared the effect of this hybrid teaching model in two rubrics:
- final exam scores; and
- student satisfaction.
Our data show that multiple choice questions exam scores were significantly higher in students that attended hybrid sessions compared to previous cohorts who attended traditional tutorial sessions. Student satisfaction was greatly increased as well, as the traditional anatomy module was transformed into a more-engaging, student-led classroom in a number of ways:
- Students get so excited when they work collectively in intriguing and tantalizing clinical cases that even the shy students get deeply engaged.
- The Paired discussion component creates a classroom environment where students feel safe and comfortable.
- The use of technology greatly increased student engagement and in-class participation and made students feel able to freely speak up in class with their peers.
Dr Steven Buckingham, Academic lead in first year Applied Medical Science, said:
“The effect of this approach on the students’ engagement and performance was quite remarkable. This use of a quasi-experimental design should be taken as a model example for data-driven teaching policy.”
First year Applied Medical Science student Maria Sasaki, said:
“The Functional Anatomy and Medical Imaging module was very interesting and engaging. The use of the PACS system helped familiarize us with the various anatomical structures we were studying faster than texts or just videos would have. The fact that we, as a tutorial group, were tasked with diagnosing the patients on the screen during tutorials was not only more engaging, but added incentive to carefully study the anatomical structures before the tutorial.”
Incorporating hybrid teaching models into the rest of the curriculum
Our next step is to incorporate this hybrid teaching model into the entire curriculum of Applied Medical Science.
My ultimate plan is to disseminate the use of this method among medical schools around the world as a teaching strategy for medical anatomy.
What advice would you give anyone embarking on a similar revision of their module?
- Once students have analysed and discussed the clinical case, show the radiological image with the correct labels of the structures and pathological features, followed by a descriptive diagram to describe in more detail the anatomopathological mechanisms.
- Do not attempt more than five clinical cases per one-hour session.
Resources used to support the teaching
Freely available resources
- Reading lists were created using mobile app teach me Anatomy
- An interactive PACS system was employed for face-to-face sessions
- High-fidelity simulators for medical professionals were employed to allow students to perform bronchoscopy and endoscopy interventions in virtual patients using their mobile phone:
- Pathological images were taken from BMJ Best practice website (not free) and from Radiopaedia (free)
Resources requiring subscription
- Online lectures showing expert dissections of cadaveric subjects were selected from Acland’s Video Atlas of Human Anatomy.
- Case studies and clinical cases were taken from the British Medical Journal Best Practice website.
Commentary from UCL Arena Centre Fellow, Dr Brent Carnell
Neph is combining multiple innovative approaches to learning, including flipping lecture content, so students have to come prepared, with interactive computer-based learning applications, among others.
Colleagues across different disciplines will be hopefully inspired by Neph’s approach of bringing in multiple learning styles, to enhance the student experience.
If a historical and traditional subject like Anatomy can be reinvigorated, then there’s no limit to what we can do.
 Close
Close

