Here you will find more information on our clinical practice.
Most disease of the pituitary and central skull base are treated surgically using the so-called endoscopic transnasal approach, in which the surgeon works through the nostrils.
The Pituitary and Central Skull Base Unit performs approximately 200 procedures every year – making it the largest centre in the UK. The unit places great emphasis on quality and safety and enjoys an international reputation, receiving many referrals from around the world.
The Unit offers neurosurgical solutions for people living with a range of diseases affecting the pituitary and central skull base. These include benign diseases such as:
- Non-functioning pituitary adenoma
- Functioning pituitary adenoma (including Cushing’s disease, acromegaly, prolactinoma, and TSHoma)
- Rathke’s cleft cysts
- Craniopharyngioma
- Meningioma
And malignant (cancerous) diseases such as:
- Chordoma
- Chondrosarcoma
- Olfactory neuroblastoma
We also provide support to surgeons caring for paediatric patients with pituitary adenoma and related diseases at Great Ormond Street Hospital for Children.
Pituitary surgery
The most common operations we perform are for pituitary disease, including pituitary adenoma. Please see the below videos for information on what the pituitary gland is, why pituitary tumours need treating, the treatment options, and the risks of surgery.
Case study
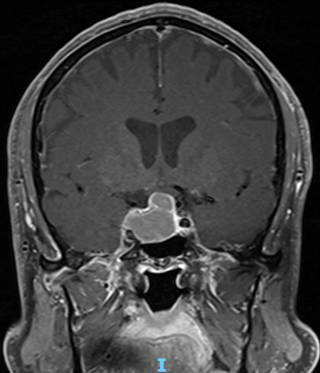
In the run-up to the 2020 outbreak of Covid-19, builder Mr H, now 63, started experiencing occasional bouts of double vision: "It was usually while watching the football, and I’d be seeing more footballs and players than were on the pitch. Then one day, I was working on two pipes under the kitchen sink at my daughter’s and I saw four instead. That’s what raised the alarm.”
Alongside this, Mr H was experiencing recurrent headaches, and both problems were initially attributed to his eyesight. Mr H tried new contact lenses, and even went on to have laser eye surgery. After the eye surgery had proved ineffective, a further examination at the eye clinic led to Mr H being admitted to UCLH where a pituitary tumour was diagnosed. While he was there, he received a visit from Hani Marcus, a consultant neurosurgeon at The National Hospital.
“Obviously when I first heard it was a tumour, I was scared,” says Mr H. “But I got talking to Hani and we’re both Arsenal supporters so we had a rapport straight away.”
Although the tumour was established as benign, Mr H remained anxious about the nature of the operation until a staff nurse talked him through the procedure.
“She sat down at the end of my bed and explained that they go in through the nose,” says Mr H. “Of course, that was reassuring, because I thought they were going to shave my head and open it up. Not only that, I found out they do four surgeries a day and the success rate for what I was having done was good - they’ve never lost anyone.”
On 10 November 2020, Mr H underwent successful neurosurgery to remove his pituitary tumour.
“I just remember opening my eyes after the operation and being able to see everything, it was bright as anything,” he says. “I healed very quickly afterwards and I can’t speak highly enough of Hani Marcus – I honestly think he saved me. And the team at Queen Square was good as gold. I have nothing but respect for them, all the nurses, everyone.”
A year after the operation, a follow-up MRI scan showed that the tumour had begun to grow back so Mr H was advised to undergo a course of radiotherapy, overseen by Karthica Indramohan, a specialist neuro-oncology radiographer with whom he had a weekly review.
"Kat said to me: ‘you’ve got a growth there that likes living where it is. I don’t think we’re going to kill it off with the radiotherapy, we just want to upset it, so it doesn’t want to live there.”
Responses to radiotherapy vary widely but Mr H was able to continue working throughout: “I had no issues at all. I went in every day for five weeks - I work in London so I could be at hospital for 8.30, have my treatment and then be back in at work an hour later.”
Mr H's most recent MRI scan was in November 2022, and he will have to wait a further three months until the impact of the radiotherapy can be seen.
“Having been through it does make you worry a bit more – so I’ve only got to get the slightest twinge or a headache and I do get a bit concerned now,” says Mr H. “But the thing is once the team at Queen Square have got you, they do not let you go, they keep an eye on you. There was no hardship, the people were pleasant. It’s all been good.”
Alex Elliott, Writer, The National Brain Appeal - Reproduced with permission from the patient
 Close
Close