New therapeutic target for rare type of childhood epilepsy
11 December 2023
Researchers at the Francis Crick Institute, UCL Queen Square Institute of Neurology and MSD have identified a potential treatment target for a genetic type of epilepsy.
Developmental and epileptic encephalopathies are rare types of epilepsy which start in early childhood. One of the most common types of genetic epilepsy, CDKL5 deficiency disorder (CDD), causes seizures and impaired development. Children are currently treated with generic antiepileptic drugs, as there aren’t yet any disease-targeting medications for this disorder.
CDD involves losing the function of a gene producing the CDKL5 enzyme, which phosphorylates proteins, meaning it adds an extra phosphate molecule to alter their function. Until now, researchers have not been sure how genetic mutations in CDKL5 cause CDD.
Through their research, published today in Nature Communications, the researchers (including Professor Gabriele Lignani and Yichen Qiu, UCL Queen Square Institute of Neurology) examined mice which lacked the Cdkl5 gene, and used a technique called phosphoproteomics to scan for proteins which are a target for the CDKL5 enzyme.
They identified a calcium channel, Cav2.3, as a target. Cav2.3 allows calcium to enter nerve cells, exciting the cell and allowing it to pass on electrical signals. This is needed for the nervous system to function properly, but too much calcium coming into cells can result in overexcitability and seizures.
The researchers then recorded from the calcium channels to see what was happening when they were not being phosphorylated by CDKL5. The channels were able to open, but were taking a lot longer to close, leading to larger and more prolonged currents flowing through them. This implies that CDKL5 is needed to limit calcium entry into cells.
The researchers also used nerve cells derived from stem cells taken from people with CDD, again observing that phosphorylation of Cav2.3 was reduced. This suggests that Cav2.3 function is potentially altered in humans as well as mice.
Mutations in Cav2.3 that enhance channel activity are already known to cause severe early onset epilepsy in a related condition called DEE69, which shares a lot of the same symptoms of CDD. These results suggest that Cav2.3 overactivity is a common feature of both disorders, and that inhibiting Cav2.3 could help with symptoms like seizures.
Sila Ultanir, Senior Group Leader of the Kinases and Brain Development Laboratory at the Crick, said: “At the moment, there’s a clear need for drugs which specifically target the biological nature of CDD. We’ve made a molecular link between CDKL5 and Cav2.3, mutations in which produce similar disorders. Inhibiting Cav2.3 could be a route for trials of future targeted treatments.”
Marisol Sampedro-Castañeda, postdoctoral researcher at the Crick, and first author, said: “Our research highlights for the first time a CDKL5 target with a link to neuronal excitability. There’s scattered evidence that this calcium channel could be involved in other types of epilepsy too, so we believe that Cav2.3 inhibitors could eventually be tested more widely.
“Our findings have implications for a large group of people, from the families affected by these conditions to researchers working in the rare epilepsy field.”
Professor Gabriele Lignani, Professor of Translational Neuroscience, Department of Clinical and Experimental Epilepsy, UCL Queen Square Institute of Neurology, said: “I believe that inhibiting Cav2.3 could be a translational target for CDD, and potentially to epilepsies with other aetiologies. This can open new avenues in the treatment of this severe pathology.”
This research was funded by MSD and the Loulou Foundation, a private foundation dedicated to the development of therapeutics and eventual cures for OCD.
Jill Richardson, Executive Director and Head of Neuroscience Biology at MSD, said: “MSD is proud of this innovative research resulting from a collaboration with researchers at the Crick and UCL. We have collectively furthered our scientific understanding of the biological targets associated with the aetiologies of Developmental Epileptic Encephalopathies – an understanding we hope will contribute toward scientific progress in this important area of high, unmet medical need.”
The researchers are now working with Lario Therapeutics, a recently launched biotech company which is seeking to develop first-in-class CaV2.3 inhibitors as precision medicines to treat CDD and related neurodevelopmental syndromes.
Links
- Sampedro-Castañeda, M. et al. (2023). Epilepsy-linked kinase CDKL5 phosphorylates voltage-gated calcium channel Cav2.3, altering inactivation kinetics and neuronal excitability. Nature Communications. 10.1038/s41467-023-43475-w.
- The Francis Crick Institute
- MSD
- Lario Therapeutics
- Loulou Foundation
- Professor Lignani's academic profile
Source: The Francis Crick Institute
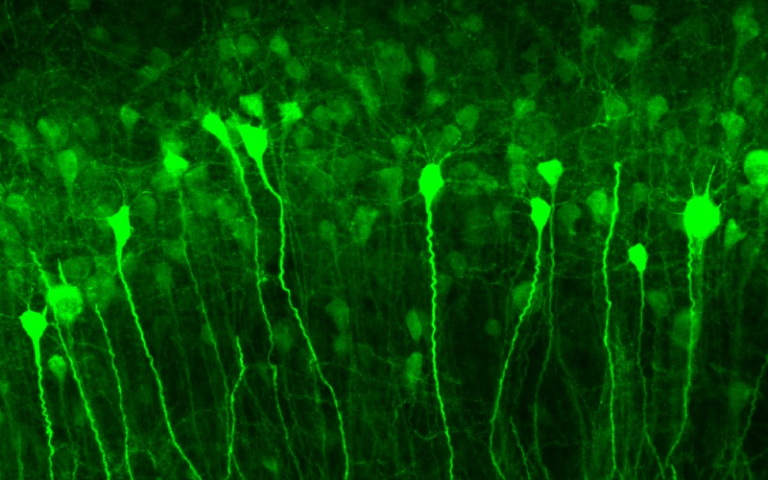
Image: When neurons participate in a seizure (green), the new gene therapy activates to tamp down their future activity. Benito Maffei / University College London
 Close
Close

