MDC Publication Highlights - March-April 2020
18 May 2020
Managing Parkinson’s advanced therapies in the time of COVID-19, Analysis of common reasons for hospitalization of people with Parkinson’s, Iron-mediated mechanism of cell death in alpha-synuclein pathologies & Discovery of new genetic cause for familial myoclonus-dystonia
Managing Parkinson’s advanced therapies in the time of COVID-19
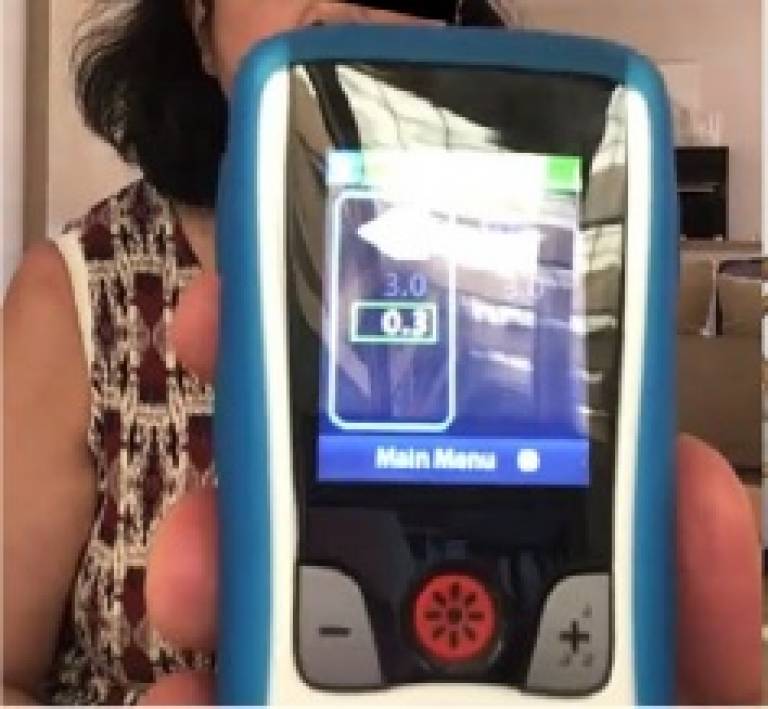
The current COVID-19 pandemic has forced health systems to rapidly change priorities in medical care, and this has had a dramatic impact on many patients with chronic conditions, including those with Parkinson’s. Restrictions on travel, cancellation of elective patient appointments and surgeries and diversion of neurology medical staff to COVID-19 hospital units have all had major impact on the care of people with Parkinson’s, in particular those requiring advanced (device-aided) treatment. There is now an urgent need for movement disorders specialist clinical services to find alternative models of care to minimize risk for this vulnerable patient population and continue to provide them with the necessary medical care and advice. In this viewpoint article, leading movement disorders neurologists from around the world are sharing their experiences and providing a common approach to the care of people with Parkinson’s, with a focus on those already on advanced therapies. This may serve as guidance for clinicians in the current pandemic and for any future emergency situations that may arise. While most neurology specialist services were unprepared to deal with the current situation, this crisis can be considered as an opportunity to change existing work schemes and encourage hospitals and health care systems to facilitate the remote management of chronic neurological patients, including those with advanced Parkinson’s.
Fasano et al. ‘Management of Advanced Therapies in Parkinson’s Disease Patients in Times of Humanitarian Crisis: The COVID-19 Experience’. Movement Disorders Clinical Practice, First Published: 20 April 2020, DOI: 10.1002/mdc3.12965.
Reasons for hospital admission of people with Parkinson’s
Parkinson's disease is the second most common neurodegenerative disease with an estimated prevalence of ~200 per 100,000 people in the UK. These figures are expected to rise quickly over the next few decades as life expectancy is increasing. While Parkinson’s can be often well managed in early stages of disease, as the disease progresses symptoms worsen resulting in increasing disability and deterioration in general health, leading to rising rates of hospital admissions. In fact, the rate of hospitalization for people with Parkinson’s is 1.4 times higher than that of other individuals in a similar age. The current study, led by MDC researcher Prof. Anette Schrag together with colleagues from the UCL department of Population Health, sought to identify the main reasons for hospital admissions in people with Parkinson’s. This investigation could help assess the gaps in care and the difficulties experienced by people with Parkinson’s and thus plan better targeted strategies to reduce hospital admissions and improve clinical outcomes. The researchers conducted a systematic review and meta-analysis of scientific publications providing reasons for hospital admission among people with Parkinson’s, covering reports of over 7,000 people in the final analysis. The most common reasons for hospitalisation among people with Parkinson’s were, in similar proportions, infections (mainly urinary tract infection and pneumonia), worsening of motor symptoms of Parkinson’s and falls or fractures. Other common reasons included cardiovascular problems associated with Parkinson’s, neuropsychiatric and gastrointestinal complications. Further research is now needed to implement targeted preventative strategies for these complications among people with Parkinson’s. Understanding and implementing preventive strategies for these key contributors to hospital admission has the potential to reduce hospital admission and thereby improve the quality of life of people with Parkinson’s and reduce burden on the healthcare system.
Okunoye et al. ‘Factors associated with hospitalisation among people with Parkinson's disease – A systematic review and meta-analysis’. Parkinsonism and Related Disorders, First Published: 28 February 2020, DOI: 10.1016/j.parkreldis.2020.02.018.
Alpha-synuclein aggregation drives cell death via iron-dependent cellular mechanism
A number of neurodegenerative diseases, primarily Parkinson’s Disease are characterised by abnormal deposits (aggregates) of a protein called alpha-synuclein in the brain. While there are strong evidence to indicate that alpha-synuclein aggregation causes Parkinson’s and related conditions, it is unknown how aggregation leads to cell death. The current study, led by MDC investigator Dr. Sonia Gandhi, used cells derived from human patients to study the effects of increased expression of alpha-synuclein and the effects of alpha-synuclein aggregation on neurons’ function, signal transmission and viability. The researchers found that clumps of alpha-synuclein directly interact with the cells’ outer membrane in a way that disrupts communication and signal transduction in neurons. Another key discovery was that alpha-synuclein aggregation induces the breakdown of lipids in the cell’s membrane (process called lipid peroxidation), and is doing so via a mechanism dependent on iron. This process induces a specific type of cell death called “ferroptosis”, and the researchers showed it can be blocked (and prevent cells from dying) by iron chelators. Thus, modulation of lipid peroxidation or iron-dependent cell death (ferroptosis) may represent new potential therapeutic approaches for Parkinson’s.
Angelova et al. ‘Alpha synuclein aggregation drives ferroptosis: an interplay of iron, calcium and lipid peroxidation’. Cell Death & Differentiation, First published: 27 April 2020, DOI: 10.1038/s41418-020-0542-z.
KCNN2: New genetic cause for familial myoclonus-dystonia
While there is a growing list of identified genes causing different types of dystonia, many familial dystonia syndromes remain without a known cause. In the current study, researchers from the UCL Institute of Neurology explored the cause of autosomal dominant tremulous myoclonus-dystonia in a UK family across three generations. The researchers combined clinical and electrophysiological investigations with detailed genetic sequencing to identify candidate causal gene variants. They identified a mutation in the KCNN2 gene, likely causing dysfunction of the respective potassium channel, as the underlying cause of the disease. This is the first time that KCNN2 mutations have been described as pathological in human disease, and further investigation in families with unexplained neurological syndromes will help establish their prevalence and full clinical spectrum.
Balint et al. ‘KCNN2 mutation in autosomal-dominant tremulous myoclonus-dystonia’. European Journal of Neurology, First published: 25 March 2020, DOI: 10.1111/ene.14228.
 Close
Close

