MDC Publication Highlights - August 2019
3 September 2019
Review of clinical features, diagnosis and emerging treatments for Hereditary spastic paraplegia, and research from The Queen Square Brain Bank identifying features that can improve clinical diagnosis of multiple system atrophy
Hereditary spastic paraplegia – clinical features, diagnosis and emerging treatments
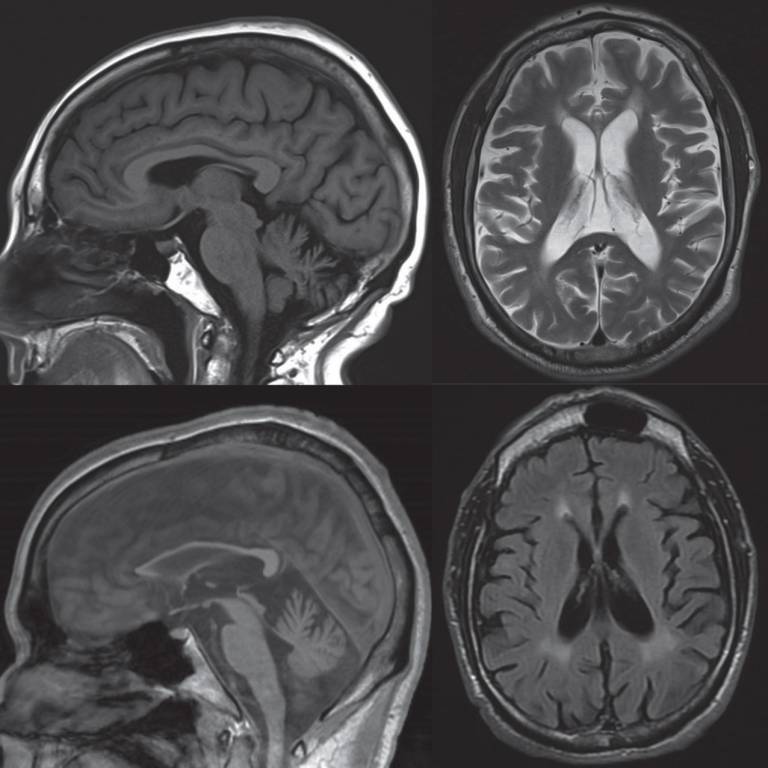
Hereditary spastic paraplegias (HSPs) is a general term for a group of rare neurodegenerative disorders characterized mainly by lower limb spasticity - a condition in which some muscles are continuously contracted. The condition can start at any age, and is usually genetic. While as many as 79 genes related to HSP have been identified, the genetic cause of the disease remains unknown in more than half of patients suspected to have HSP. This article reviews the more common HSPs encountered in clinic and suggests a diagnostic approach highlighting clinical features, neuroimaging and neurophysiological findings. The authors, led by MDC clinician-researcher Prof. Tom Warner, also discuss management strategies, focusing on emerging therapeutic options for some specific HSPs based on their underlying genetic causes and molecular mechanisms.
Shribman et al. ‘Hereditary spastic paraplegia: from diagnosis to emerging therapeutic approaches’. The Lancet Neurology, First published: 31 July 2019, DOI: 10.1016/S1474-4422(19)30235-2.
Improving diagnosis of multiple system atrophy
Multiple system atrophy (MSA) is an adult-onset, rapidly progressing, fatal neurodegenerative disease. Clinical diagnosis of multiple system atrophy is challenging and many patients are misdiagnosed with other conditions such as Lewy body disease or progressive supranuclear palsy. A definite diagnosis of MSA requires post-mortem neuropathological confirmation, and neuropathological studies indicate that as many as 1 in 3 patients are misdiagnosed in life. In the current study, researchers from the Queen Square Brain Bank at the UCL Institute of Neurology, reviewed the clinical records of 203 patients with a clinical diagnosis of MSA and subsequent neuropathological investigation to identify diagnostic pitfalls and clinical features that could improve the accuracy of clinical diagnosis. The researchers found that clinical establishment of autonomic dysfunction combined with the presence of a combination of seven specific “red flag” features, were highly specific markers distinguishing MSA from other similar conditions.
Miki et al. ‘Improving diagnostic accuracy of multiple system atrophy’. Brain, First published: 9 July 2019, DOI: 10.1093/brain/awz189.
 Close
Close

