MDC Publication Highlights - September 2019
9 October 2019
Can a shorter pulse-width reduce negative effects of DBS in Parkinson’s?, Automatic brain image analysis tool to aid diagnosis of Atypical parkinsonism & Review of Myoclonus-dystonia syndromes
Can a shorter pulse-width reduce negative effects of Deep Brain Stimulation in Parkinson’s?
Deep Brain Stimulation (DBS) of the subthalamic nucleus is a well-established treatment for improving motor symptoms in people with Parkinson’s. However, long term DBS treatment may worsen some symptoms of Parkinson’s, most notably causing a deterioration of speech intelligibility. MDC researchers, led by Prof. Tom Foltynie, investigated whether using a shorter pulse-width for the stimulation could reduce the negative side effects of DBS, while maintaining its beneficial effecs. The researchers conducted a pilot clinical trial, which looked at the effects of applying a shorter pulse width stimulation in patients who have been treated with standard DBS for 2-12 years and have developed moderate speech problems. Overall the trial indicated that using a shorter pulse width had similar therapeutic effects as standard stimulation. Researchers also observed that a shorter pulse width might improve speech intelligibility, but only if introduced early in the course of DBS treatment. This work indicated that there is scope for conducting larger clinical trials exploring potential benefits of short pulse width over conventional stimulation settings, specifically in patients who develop dysarthria early in the course of their DBS treatment.
Dayal et al. ‘Short Versus Conventional Pulse-Width Deep Brain Stimulation in Parkinson’s Disease: A Randomized Crossover Comparison’. Movement Disorders, First published: 30 September 2019, DOI: 10.1002/mds.27863.
Automatic brain image analysis tool to aid diagnosis of Atypical parkinsonian syndromes
Atypical parkinsonian syndromes are a group of conditions (including progressive supranuclear palsy, corticobasal syndrome and multiple system atrophy) which often resemble Parkinson’s disease upon initial presentation but are characterized by additional features not typical for PD as well as a more rapidly progressing and debilitating disease course. While there are currently no curative treatments for atypical parkinsonism, potential disease-modifying therapies are in development and it is therefore critical to develop better ways of accurately diagnosing these conditions early in the disease course. One potential diagnosis methods is “brainstem segmentation”: using MR imaging to compare the size/volume of specific sub-regions within the brainstem. The current research, led by MDC researcher Prof. Huw Morris and colleagues from the UCL Institute of Neurology, sought to evaluate whether an automatic computerized segmentation tool could generate reliable segmentation data that would be informative for diagnosis of different atypical parkinsonian conditions. The researchers found that the automated segmentation method was able to accurately measure the different brainstem components and to quantify their involvement in atypical parkinsonian syndromes. The method was able to detect specific patterns of brainstem pathology unique to each condition, making it a viable tool to aid clinical diagnosis.
Bocchetta et al. ‘Automated brainstem segmentation detects differential involvement in atypical Parkinsonian syndromes’. Journal of Movement Disorders, First published: 26 September 2019, DOI: 10.14802/jmd.19030.
Clinical features and molecular mechanisms of Myoclonus-dystonia syndromes
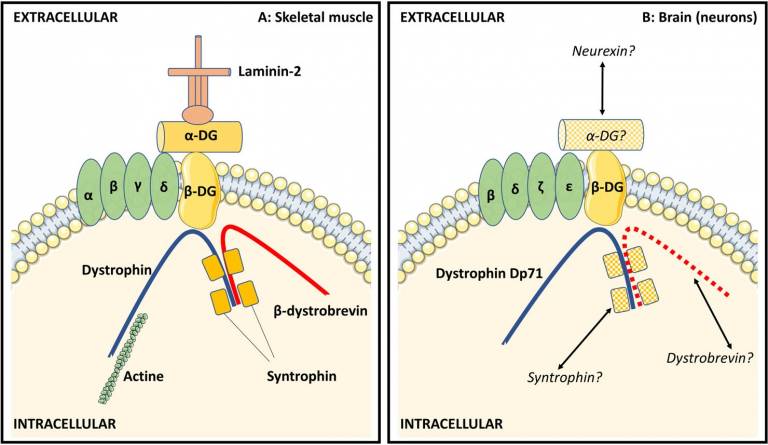
Myoclonus-dystonia is a very rare syndrome typically beginning in childhood and characterized by myoclonic jerks and dystonia involving the neck, trunk, and upper limbs. Myoclonus-dystonia is a genetic condition, most commonly resulting from mutations in the epsilon-sarcoglycan (SGCE) gene. Subsequent to the identification of SGCE, additional genes have been found to cause syndromes similar to SGCE-related myoclonus-dystonia, and are thus considered part of a spectrum of myoclonus-dystonia syndromes. In this articles, researchers led by Prof. Kailash Bhatia from UCL MDC describe the clinical presentation of myoclonus-dystonia syndromes, including neurophysiological findings and current therapeutic options. The authors also discuss the genetic determinants of myoclonus-dystonia syndromes and the molecular mechanisms involved in the pathophysiology of these syndromes.
Menozzi et al. ‘Twenty Years on: Myoclonus-Dystonia and ε-Sarcoglycan — Neurodevelopment, Channel, and Signaling Dysfunction’. Movement Disorders, First published: 26 August 2019, DOI: 10.1002/mds.27822.
 Close
Close

