Our academic work is split between three sites: Institute for Women’s Health (incorporating UCLH), the National Hospital for Neurology and Neurosurgery and the Microbiology Department at the Eastman Dental Institute. The studies carried out at each site are briefly outlined within each site.
EGA Institute for Women's Health
Chronic LUTS - Microbiology Unit at the Eastman Dental Hospital
Neuro-Urogynaecology, Pain Medicine and Neuromodulation - The National Hospital for Neurology & Neurosurgery
EGA Institute for Women's Health
Our main research work at this site undertakes to investigate three unique issues affecting women in the UK today suffering with pelvic floor dysfunction. They include:

Research Projects:
Quality of Life outcomes after mesh removal | CI: S Elneil Study Type: Quantitative Funding: Charity |
Patient experience with mesh complications | CI: S Elneil Study Type: Qualitative Funding: Charity |
Recurrent Urinary Stress Incontinence and Prolapse after Mesh Removal: Native Tissue Repair Outcomes | CI: S Elneil PI: G Vorona Study Type: Quantitative Funding: Charity |
Research Project:
Quality of Life outcomes after treatment for Chronic LUTS | CI: R Khasriya Study Type: Quantitative and Qualitative studies Funding: Charity |
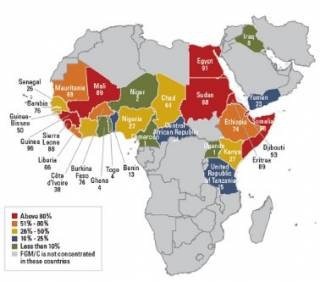
Female Genital Mutilation (FGM) is an extreme form of gender-based violence that affects at least 200 million women and girls worldwide1. Four main types of FGM are
recognised by the World Health Organization (WHO), with Types I and II accounting for approximately 80% of all cases. Although the matter of safeguarding young girls is now well-recognised, and adhered as well as criminalised in many countries, the long-term impact on the pelvic floor is not well established. There are significant risks of chronic urinary/vaginal infections, chronic pain, gynaecological and obstetric complications, as well as life-long emotional, psychological, and sexual problems. FGM can still result in fatalities. What is more, carrying out FGM constitutes a violation of girls’ and women’s rights. The FPMRS team have been carrying out research in this group of women since 2015.
Research Projects - Prevalence of FGM in UK
Urogynaecology symptoms in women with FGM | CI: S Elneil PI: I Siddig and Y Saruchera Study Type: Quantitative Funding: HCA & Charity |
Chronic LUTS - Microbiology Unit at the Eastman Dental Hospital
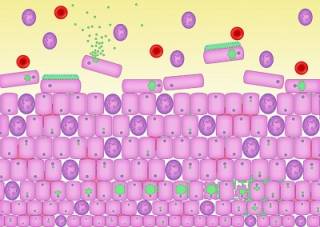
How urinary pathogens become embedded in the epithelium of the bladder. Malone-Lee et al.

Neuro-Urogynaecology, Pain Medicine and Neuromodulation at the National Hospital for Neurology and Neurosurgery
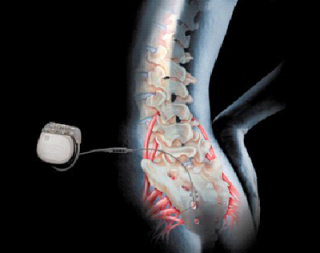
These three disciplines are based within the Department of Uro-neurology at the National Hospital for Neurology and Neurosurgery, Queen Square, and the Pain Management Centre on Cleveland Street. The academic work on neuromodulation and neuro-urogynaecology includes:
Neuromodulation in Women
Research Projects:
| Long term Quality of Life Outcomes in women with chronic urinary retention | CI: S Elneil Study Type: Quantitative Funding: Charity |
Quality of Life outcomes after neuromodulation in women with hypermobility disorders | CI: S Elneil PI: A Baha Khan Study Type: Quantitative Funding: HCA and Charity |
Sensory dysfunction in the bladder pre- and post-neuromodulation | CI: S Elneil Funding: Charity |
Innovative Neuromodulation
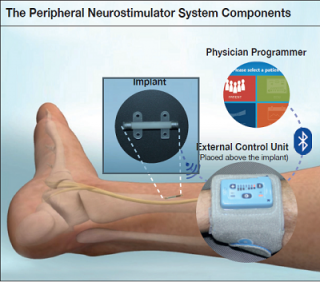
Tibial nerve stimulation (TNS) is the least invasive form of neuromodulation used to treat associated symptoms of urinary urgency, urinary frequency and urge incontinence has been shown to reduce OAB symptoms. It involves sending electrical stimulation through the tibial nerve, located in the lower leg, to the bladder to control OAB symptoms. One of the shortcomings of the current therapy available is the weekly clinic visits for the first 3 months, and thereafter 2-8 weekly visits for ‘top-up’ sessions of treatment. Bluewind Medical has developed an implantable tibial nerve stimulator which can be used at home, thus eliminating the necessity of frequent visits to the clinic. They successfully completed the safety trial in 2018. The FPMRS team are currently part of a national and international study looking its efficacy in bladder dysfunction.
Research Projects:
Bluewind Medical Trial: Role of implantable tibial nerve modulators in overactive bladder | CI: S Elneil (3 UK sites and 7 European sites) Funding: Commercial |
Saluda Medical: Electrical assessment of sacral nerves in patients, using electrophysiology | CI: C Knowles (Queen Mary University) PI: S Elneil Funding: Commercial |
Chronic Pain in Women
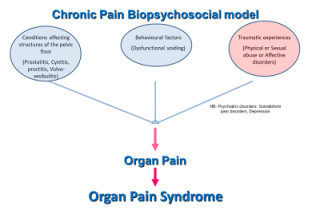

Chronic pelvic pain syndrome is the occurrence of CPP when there is no proven infection or other obvious local pathology that may account for the pain. It is often associated with negative cognitive, behavioural, sexual, or emotional consequences, as well as with symptoms suggestive of lower urinary tract, sexual, bowel or gynaecological dysfunction. Chronic Pelvic Pain Syndrome is a sub-division of CPP. This forms the basis the biopsychosocial model of chronic pain.
Many women with chronic pain often have a bladder component, and on cystoscopic assessment petechial haemorrhages may be seen.
Research Projects:
Chronic Pain in Mesh complications | CI: S Elneil PI: M Stasiowska Study Type: Qualitative and Quantitative Funding: Charity |
Chronic Pain and Chronic LUTS | CI: R Khasriya Study Type: Qualitative and Quantitative Funding: Charity |
Neuromodulation in Chronic Pain | CI: S Elneil PI: A Shetty Study Type: Qualitative and Quantitative Funding: Charity |
Botulinum Toxin Therapy in Women
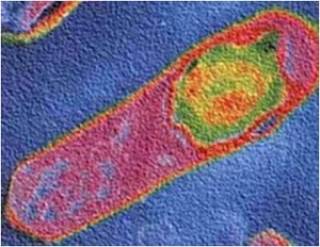
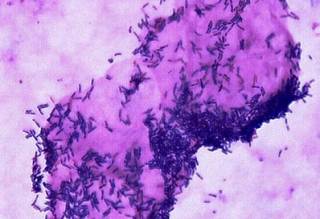
Clostridium botulinum bacteria ®Allergan
In 2000, botulinum toxin treatment to the bladder in neuropathic DO was reported in the literature. Botulinum toxin (abbreviated either as BTX or BoNT and usually known as Onabotulinum toxin A®) is produced by Clostridium botulinum, a gram-positive anaerobic bacterium. The successful reduction in the debilitating symptoms of urgency, urge incontinence, and frequency was hugely significant in patient’s lives. This therapy is now licenced for widespread use in all patients with overactive bladder, who had failed or could not tolerate pharmacotherapy.
Neuro-urogynaecology Research

We study the dysfunction of the pelvic floor in patients with well-defined neurological disorders such as Multiple Sclerosis or Parkinson’s Disease. We also study pelvic floor dysfunction, where no known cause is determined, but for which chemo- or electrical neuromodulation may be helpful. These include conditions such as voiding dysfunction, chronic urinary retention, primary/secondary failure of sphincter relaxation, pelvic pain states, hypermobility states and sacral neuropathy.
 Close
Close

