In each year of your degree you will take a number of compulsory modules. Modules are assessed in the academic year in which they are taken through both formative and integrated summative methods.
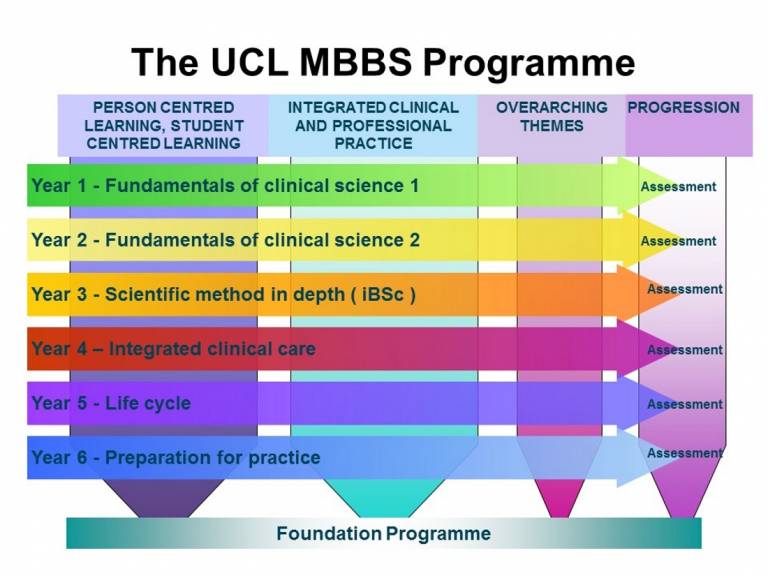
Your degree will follow a six-year programme inclusive of an integrated BSc (except for graduate entrants with UK degrees who are exempt) leading to the award of the Bachelor of Science (BSc) and Bachelor of Medicine and Bachelor of Surgery (MBBS). Highly motivated students who are aiming for a career in academic medicine may apply for the MBPhD programme which is taken between years 4 and 5 of the MBBS programme.
The MBBS programme aspires to educate the 'UCL Doctor': a highly competent and scientifically literate clinician who is equipped to practise patient-centred medicine in a constantly changing modern world and has a foundation in the basic medical and social sciences.
The MBBS at UCL is a six-year integrated programme of study. Each year is comprised of a number of themed integrated modules with Clinical and Professional Practice modules running vertically through the programme and Student Selected Components in Years 1, 2 and 6.
Year 1: Fundamentals of Clinical Science 1
Year 2: Fundamentals of Clinical Science 2
Year 3: Integrated BSc
Year 4: Integrated Clinical Care
Year 5: The Life Cycle and Specialist Practice
Year 6: Preparation for Practice
- Year 1: Fundamentals of Clinical Science 1
Fundamentals of Clinical Science (Years 1 and 2) provides an underpinning learning experience in basic clinical sciences and the foundations of learning in the vertical themes that run through all years of the curriculum.
Systems based learning is delivered as a series of sequential, integrated, systems based modules.
Each module:
- is based around a physiological system;
- provides integrated teaching across disciplines;
- is integrated with the learning within the vertical modules;
- and is designed to build on knowledge and skills learnt in previous modules.
There are opportunities for early patient contact and for meeting health professionals, to allow you to keep preparation for the practice of medicine firmly in sight.
The aims of the Fundamentals of Clinical Science years are for you to:
- gain a firm understanding of the scientific knowledge and principles that are relevant to, and essential for, excellence in clinical practice;
- develop an understanding of science in the context of its application to clinical medicine, organised according to physiological and functional systems (e.g., Circulation and Breathing), rather than by academic disciplines (e.g., physiology, biochemistry and anatomy);
- understand the application of science to medicine and have the skills to appreciate the methods of scientific research, thereby enabling you to appreciate and understand future advances in medicine;
- gain a good foundation for the integrated BSc in Year 3;
- develop the key skills required for data collection and analysis, information retrieval and use of electronic databases, problem solving, report writing and presentation of information and case reports;
- have opportunities to appreciate the ethical, social and legal dimensions of medicine;
- have an opportunity for early patient contact and start to develop the foundations of the professional skills required for good patient care;
- start to develop an understanding of the value of health education, preventive medicine and the natural history of disease;
This will be achieved in Year 1 through:
- an Introduction and Orientation Module to Year 1;
- a Foundations of Health and Medical Practice Module, to provide essential core systems knowledge and an introduction to learning in medicine;
- systems based learning in horizontal modules: Infection and Defence, Circulation and Breathing, and Fluids, Nutrition and Metabolism that occur in sequential blocks during the year;
- CPP modules that are ongoing throughout the year and extend into the latter years of the programme;
- three Consolidation, Integration and Feedback weeks;
- formative assessments throughout the year, including an Objective Clinical and Practical Examination (OCaPE);
- maintenance of a portfolio and practical procedures checklist;
- written and a practical (OCaPE) summative assessment towards the end of the year;
- Year 2: Fundamentals of Clinical Science 2
Like year 1, learning is presented as a series of sequential, integrated, systems based modules.
Each module is based around a physiological system, provides integrated teaching across disciplines, is integrated with clinical and professional practice (CPP) and is designed to build on knowledge and skills learnt in previous modules.
There are opportunities for early patient contact and for meeting health professionals, to allow you to keep preparation for practice firmly in sight.
The aims of both of the Fundamentals of Clinical Science years are for you to:
- gain a firm understanding of the scientific knowledge and principles that are relevant to, and essential for, excellence in clinical practice;
- develop an understanding of science in the context of its application to clinical medicine, organised according to physiological and functional systems (e.g., endocrine system), rather than by academic disciplines (e.g., physiology, biochemistry and anatomy);
- understand the application of science to medicine and have the skills to appreciate the methods of scientific research, thereby enabling you to appreciate and understand future advances in medicine;
- gain a good foundation for the knowledge and skills required for the integrated BSc in Year 3;
- develop the key skills required for data collection and analysis, information retrieval and use of electronic databases, problem solving, report writing and presentation of information and case reports;
- have opportunities to appreciate the ethical, social and legal dimensions of medicine;
- have an opportunity for early patient contact and start to develop the foundations of the professional skills required for good patient care;
- start to develop an understanding of the value of health education, preventive medicine and the natural history of disease;
This will be achieved in Year 2 through:
- systems based learning in modules: Movement and Musculoskeletal Biology; Neuroscience and Behaviour; Endocrine Systems and Reproduction; Genetics, Development and Cancer; that occur in sequential blocks throughout the year;
- CPP modules that build on learning in Year 1 and are ongoing throughout the year and extend into the latter years of the programme;
- relating learning where appropriate to the UCL MBBS core conditions and presentations;
- the patient pathways: continuing with the Integrated and community care patient pathway and a cardiometabolic patient pathway, including extended patient contact with patients who have cardiometabolic disorders;
- formative assessments throughout the year, including an Objective Clinical and Practical Examination (OCaPE);
- maintenance of a portfolio including the record of completed procedures card;
- written and a practical (OCaPE) summative assessment;
- Year 3: Integrated BSc
The Medical School offers a wide range of 1 year integrated BSc programmes. UCL medical students, except those who are already UK graduates, are required to take an integrated BSc as a compulsory part of their 6 year MBBS programme after completion of Year 2 of the MBBS.
The multi-faculty, multi-disciplinary structure of UCL means that we are in a strong position to offer a wide range of degree programmes of a high academic standing.
During the BSc year, students have the opportunity to study topics in greater depth than during their medical studies. It also affords them the opportunity to become familiar with research literature, scientific methods and techniques and the current state of thinking in their selected area. This is a very valuable experience and will help you to determine your aptitude and enthusiasm for future research in your clinical career.
- Year 4: Integrated Clinical Care
This year aims to integrate knowledge of the clinical sciences into clinical practice and, by utilising extensive clinical practice and workplace based learning, in conjunction with formal teaching sessions, it also allows further development of the Clinical and Professional Practice themes and builds on the systems-based modules of years 1 and 2.
The year is divided into four parts: a short Foundation of workplace based and patient centred learning course followed by three long attachments based in hospitals and associated community and GP settings.
During the year you will focus on core presentations and the three broad categories of clinical care: community based care, ward based care and emergency care.
In each attachment you will have a substantial period within a hospital to begin to know your teachers and the healthcare teams and how the hospital works. You will have opportunities to learn from patients and clinicians in the broad areas of medicine and the general medical specialties and interventions including surgery and anaesthesia.
The theme of Year 4 is ‘integrated clinical care’. The aims of this year are to:
- help you to learn from healthcare experiences;
- become skilled at interviewing and examining patients with a range of problems across the range of healthcare settings;
- become familiar with the ways in which patients access the healthcare system and the pathways of care for a range of common presentations;
- understand the integrated approach to diagnosing and managing patients’ problems;
- safely and clearly document information about patients and their care in a clinical notes system;
The year is not focused on rotating through as many specialties as possible, but instead about spending time in longer, more generic and integrated attachments to better understand illness prevention, presentation and management.
You will have further learning opportunities in many of these specialities in year 5 and particularly year 6 so do not feel that year 4 is only about learning about the medical and surgical specialities.
It is about learning how to learn in the clinical setting and becoming experienced in having consultations with patients, eliciting medical histories and examining patients. However, you will see some specialist services and patients with rare conditions during the modules and you should make the most of these unique learning opportunities that you might not see again until you are qualified.
Year 4 is also a time when you will be both looking backwards: to your past learning, and understanding how theory and understanding of health and disease links to practice; and forwards: using the learning in this year as a key part of your journey to becoming a Foundation doctor.
By the end of Year 4 you should:
- be an excellent workplace learner: being able to make the most of experiential learning opportunities;
- understand how the NHS works and the roles of a range of healthcare providers within it;
- understand how a range of common diseases present and are managed in both community and hospital settings;
- be able to communicate comfortably and effectively with patients;
- have developed a wide range of clinical skills and be able to carry out practical procedures competently;
- be able to use the information gathered from patients, together with your developing understanding of medicine, to produce a differential diagnosis and problem list;
- be proficient in undertaking and presenting a full medical clerking (history, examination, differential diagnosis, problem list and management plan);
- Year 5: Life Cycle and Specialist Practice
The theme of Year 5 of the MBBS curriculum is “the life cycle” - you will encounter patients with medical conditions from across the “seven ages” of man. A large part of the year is dedicated to beginnings of life, through women’s and men’s health, sexual health and child health.
In addition you will learn about family and adult health and behaviour through general practice, breast services, urology, psychiatry, dermatology, ophthalmology and ENT. The latter parts of the life cycle will be explored in health of the older person, oncology and palliative care.
The year begins with an Introduction and Orientation Module (IOM) where you will be introduced to important details of the year, some core lectures covering key concepts for the year.
As Year 5 is also an important year with regards to your Foundation School application and planning your elective, within the IOM you will also receive advice about career planning, Foundation School application and arranging your elective.
The rest of the year consists of a Taught Revision week, and three modules; each module comprising a core introductory teaching week, and then 12 weeks of clinical placement.
The three Year 5 modules are:- Module A - Child and Family Health (Child Health, Core General Practice);
- Module B - Women’s Health and Men’s Health (Breast, Dermatology, Obstetrics & Gynaecology, Sexual Health & HIV Medicine, Urology);
- Module C - Health of the Older person (Cancer Medicine, Care of the Older Person, Ophthalmology, Palliative Care, Psychiatry)
- Year 6: Preparation for Practice
In the final year of the MBBS programme at UCL, students will be encouraged to integrate their prior learning in biomedical and human sciences with all their clinical experience and apply it to management during longer attachments. By ensuring that students think and act like doctors, they will learn to master key practical procedures in real clinical settings, as well as demonstrating impeccable patient-centred professionalism.
Our final year will place patient-based student led learning at its heart. Incorporating assistantships, it will be intellectually demanding and ‘hands-on’, creating UCL graduates who will become knowledgeable, decisive and practical doctors, able to work in teams and aware of patients’ needs and their own limitations.
The aims of your final year:
The MBBS Final Year is designed to ensure you have opportunities to think and act like a doctor and to practise and reflect on the areas that will be of use to you on becoming an FY1 doctor.
Thinking like a doctor:
- You should aim to make evidenced-based clinical decisions that promote patient-centred practice. You will integrate and synthesise prior knowledge of biomedical and human sciences to enhance your interpretation of the patient’s own narrative, physical signs and other clinical and social data.
Acting like a doctor:
- You should be able to demonstrate your professionalism through commitment, time keeping, initiative, respect for colleagues, an understanding of patient safety and the application of ethical and legal principles. You will be able to perform general clinical tasks and specific practical and clerical procedures (including BLS & prescribing) to the level expected of a Foundation Doctor.
- Clinical and Professional Practice (CPP)
Clinical and Professional Practice is all about helping you to become a great UCL doctor. It's delivered in all years of the MBBS programme and makes up around 20% of the curriculum and its assessments.
Clinical and Professional Practice (CPP) learning take place in several ways: lectures, small group work, placements, reflection, and online. As you move through the years from 1 to 6 CPP is increasingly integrated into the wider curriculum as it's all about how to:
- Communicate well with patients and colleagues.
- Use evidence and data wisely.
- Behave ethically, legally, and with kindness.
- Consider how patients feel when they are ill.
- Learn how our body is structured, do procedures well, and interpret imaging.
- Reflect on your own behaviour and experiences.
- Think about the 'big picture' of society, mental health, and keeping patients safe.
The 16 CPP modules are organised into three groupings:
- Integrated Clinical and Professional Practice (Anatomy and Imaging; Clinical Skills and Practical Procedures; Doctor as Data Scientist; Pathological Sciences; Use of Medicines).
- Overarching Themes (Clinical Communication; Ethics and Law; Mental Health; Patient Safety and Patient Experience; Professionalism; Social Determinants of Health).
- Student-Centred Learning, Person-Centred Learning (the Patient Pathways; the Portfolio).
The Individual Clinical and Professional Practice modulesThis contains a brief overview of the 16 CPP modules.
The synopses and Intended Learning Outcomes (ILOs) of these modules can be viewed on the MBBS Curriculum Map.Integrated Clinical and Professional Practice
The five modules in the Integrated CPP grouping address factual knowledge connecting science and clinical medicine with core skills and competencies.
Anatomy and Imaging
Working knowledge of normal and abnormal human structure and function with an ability to interpret using modern medical imaging.
Clinical Skills and Practical Procedures
Ensure you are competent and confident to perform the skills and procedures listed in the General Medical Council’s Outcomes for Graduates 2018 document.
Doctor as Data Scientist
Skills to access, understand and evaluate research evidence to use it in decision making and clinical practice and to introduce the concepts of digital health and data-driven technology.
Pathological Sciences
An understanding of the theory and application of pathological sciences to clinical diagnosis and treatment.
Use of Medicines
Knowledge of how to use the right drug, at the right dose and duration, for the right patient, whilst understanding competing aspects of pharmacology, including economic factors.
Overarching Themes
Overall Themes represent themes that either pervade all elements of practice, or are central aspects of learning in all modules.Clinical Communication
Effective communication. Recognise workplace based teaching around real patient encounters as a process of integrative thinking.
Ethics and Law
Develop core skills and an orientation for effective communication, ethical practice, and working within the framework of the law and professional guidance.
Mental Health
Enables you to gain a better understanding of mental health and be more able to help those with mental health needs, regardless of which specialty you ultimately pursue.
Patient Safety and Patient Experience
Examine the co-ordinated efforts to prevent harm to patients within healthcare. Through openness and transparency, communication and empathy, we aim to deliver a safe, patient-centred clinician.
Professionalism
Understand contemporary thinking and frameworks about what constitutes professionalism and professional practice.
Social Determinants of Health
Discuss the powerful effects of the social environment and social processes on health and illness. This is studied in relation to economic and public health policies and also at an individual level through access to, and delivery of, healthcare in local communities.
Patient-Centred Learning, Student-Centred Learning
This grouping focuses on making sense of learning, both learning over the entire programme and patient-based learning. The patient pathways also create opportunities to understand the experience of illness from the patient perspective.
Portfolio
Encourages you to take responsibility and reflect on learning and experience in order to prepare for higher training and revalidation.
Cancer Patient Pathway (Year 4)
Gaining understanding of the diagnosis and management of cancer patients, exposure to the patients’ experience of their cancer journey, and practice in forming relationships with patients.
Cardiometabolic Illness Patient Pathway (Year 2)
Meeting patients with either cardiovascular or diabetic disease. Develop skills in eliciting a history from a patient and consider investigations used in diagnosis. It also explores the impact of illness on patients and their families.
Integrated and Community Care Patient Pathway (Years 1 & 2)
Provides you with opportunities to learn from members of the public, as well as a range of health and social care providers, by sending you into the community and by bringing the community into the Medical School.
Develop your understanding of your own and of other people’s lives and to aid contemplation of the influences on and effects of health and illness, including the social and economic context of health and wellbeing or ill health and vulnerability.
Person-Centred Care Patient Pathway (Year 5)
Designed to allow you to gain insight into the patient perspective of navigating encounters with different health professionals and different healthcare settings.
- Student Selected Components (SSCs)
Students may choose Student Selected Components (SSCs) in years one, two and six and in the elective period in year six. SSCs allow students to pursue special interests and develop a range of generic skills. They include choices in science, research, the arts, and humanities and languages.
 Close
Close

