Health~Holland's Quadruple Helix Approach To Missions

22 July 2021
What is the context for the Health~Holland?
Despite the Netherlands having a robust health system that offers healthcare to all its citizens at an affordable rate, two trends have been increasing pressure on Dutch lawmakers to implement reforms. First, socioeconomic differences in health are large and persistent: between the highest and lowest socioeconomic groups there exists a six-year difference in life expectancy and a 15- year difference in healthy life expectancy. Second, the health sector’s landscape is changing with the rise of unrecognised household care activity, representing a decoupling between formal and informal systems. Indeed, much of the country’s care economy is done by relatives or friends, who are not remunerated accordingly. As a result of these socioeconomic differences and the rise of informal health sector activity, the Dutch government sought to take a proactive approach to health reform through innovation.
It is also important to understand the Netherlands’ institutional landscape around innovation. In 2011, the Dutch government created nine so-called ‘top sectors’ or economic areas that are key to the country’s economy: agriculture, horticulture, logistics, high-tech systems and materials, life sciences and health, chemicals, creative industry, energy and water. Initially, these top sectors were intended to reform the funding of innovation activities and grant Dutch companies access to global markets. In 2017, however, following the general election, the new Dutch cabinet decided the top sectors could be repurposed and restructured to contribute to societal challenges. This repurposing of top sectors into missiondriven institutions led to two significant changes. First, the agendas and roadmaps of each top sector, which had formerly been separate, became aligned into four grand societal challenges. Second, the top sectors moved from a triple helix innovation model to a quadruple helix, ensuring citizen representation.
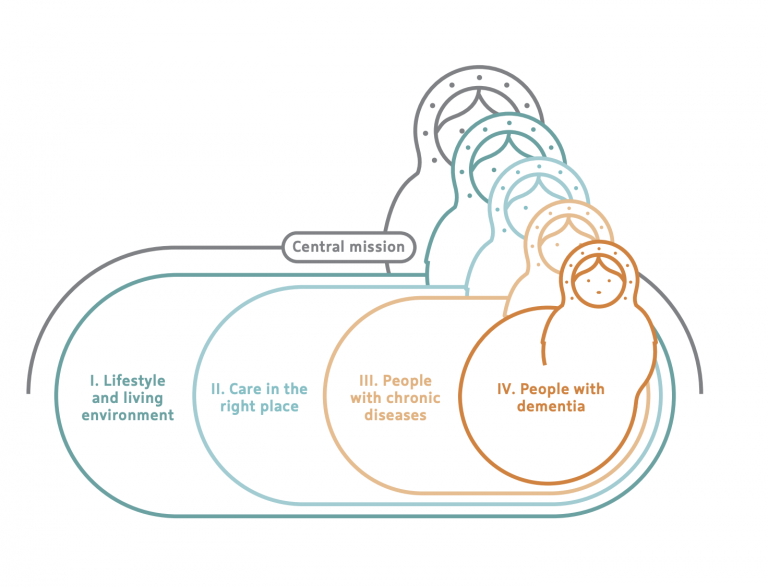
In keeping with this thinking, in 2019 the Ministry of Economic Affairs and Climate Policy supported the pre-mentioned challenges: energy transition and sustainability; agriculture, water and food; security; and health and care. The Ministry of Health, Welfare and Sport was the political body that presided over the health and care challenge and was tasked with developing one central mission and four sub-missions that would contribute to it (see Figure 1).
What was the approach to Mission-Oriented Innovation?
Health~Holland therefore conducted internal and external consultations with three different departments in the health ministry — prevention, health and cure — as well as with civil society representatives, businesses and key national health institutes. As a result of these consultations, by the end of 2019 the following central mission and four sub-missions were developed:
Central mission: By 2040, all Dutch citizens will live at least five years longer in good health, while the health inequalities between the lowest and highest socioeconomic groups will have decreased by 30%.This mission encompasses:
1. Lifestyle and living environment: By 2040, the burden of disease resulting from an unhealthy lifestyle and living environment will have decreased by 30%.
2. Care in the right place: By 2030, the extent of care will be organised and provided to people 50% more (or more often) than at present in one’s own living environment (instead of in healthcare institutions), together with the network around them.
3. People with chronic diseases: By 2030, the proportion of people with a chronic disease or lifelong disability who can participate in society according to their wishes and capabilities will have increased by 25%.
4. People with dementia: By 2030, the quality of life of people with dementia will have improved by 25%.
Once the missions were agreed upon, Health~Holland worked with other top sectors to develop the Knowledge and Innovation Covenant (KIC) 2020- 2023, a commitment by public and private sector actors to support a funding programme that will drive and sustain the various missions over their first four years. Health~Holland worked with 100 coalition partners, including representatives from civil society, industry, knowledge institutions and ministries to establish KIC. The commitment brings together investments in innovation from more than 2,200 companies, knowledge institutions and government bodies. A total of €4.9 billion has been allocated; €1.06 billion has been allocated to the Health and Care challenge, of which €525 million comes from private funding and €534 million comes from public funding. With this budget, Health~Holland has the ability to direct innovation through strategically aligned public-private partnerships.
What solutions are emerging from the missions approach?
1. Public-private partnerships and projects
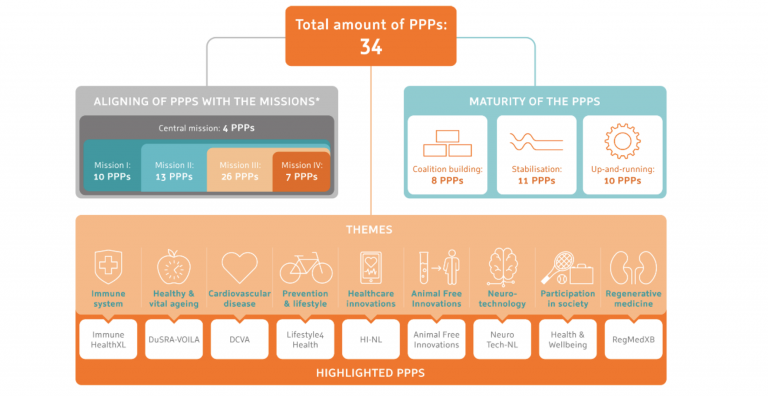
Public-private partnerships (PPPs) that Health~Holland funds are national, multi-year, thematic and programmatic collaborations between quadruple helix organisations that contribute to at least one of the five health and care missions. As of mid-2021, Health~Holland supported 34 different PPPs, most of which are either up-and-running or whose governance models and funding streams are currently being stabilised.
What, however, makes these PPPs unique? First, each of them has the capacity to bring a diversity of public and private sector actors, as well as universities and civil society representatives, together to build an innovation ecosystem around a specific challenge. Second, each PPP is mission-driven, meaning they can set their own targets and mobilise funding in service of those targets. Importantly, funding comes from both the public and private sectors.
2. Field labs (GROZzerdammen)
Working at a deeper citizen level, the Health~Holland team has established a number of GROZzerdammen: field labs in a local neighbourhood, district, municipality or village community. GROZzerdammen work on the missions by restructuring the prevention and care pyramid, from third-line care and relationships with the social domain to healthy living and informal care. These field labs offer a workspace for joint experimentation with integrated social and technological innovations. This is done in various real living environments, in urban and rural areas.
A powerful field lab example is TanteLouise, a health care organisation for people with dementia. In one TanteLouise care home, citizens, businesses, entrepreneurs and council members came together in a ‘system in the room’ process. All actors shared their dreams for the care sector, such as the desire for patients to have a meaningful life and to significantly diminish the frustration of having dementia. By sharing this dream with all systems actors, specifically in the TanteLouise home, where people with dementia actually live, the co-creation process started to address how the community can help people with dementia. The outcome was a commitment to an open village in which all residents with dementia can live in freedom, co-created by a community, enabled by technology.
“Health~Holland plans to have four to six field labs running by 2022.
3. Illustration projects
Illustration projects are another key tool in the Health~Holland missions toolkit. An illustration project is a unique and innovative idea, which will be commonplace within the next 20 years. In Health~Holland’s context the emphasis is on reducing inequality and a strong example of an Illustration project is the Ontwikkelplek van de Toekomst (Development Place of the Future). This project focuses on education and what schools should look like in the future.
According to the Onderwijs Alliantie, the school of the future requires changes in the ecosystem around children and needs to include an environment bigger than just the school as a building. This includes schools widening their interactions with communities and local actors, while focusing more on children’s talents, interests and competencies
What challenges does the Health~Holland face?
Health~Holland is aware of two main challenges going forward. First, the evaluation and measurement of each of the mission targets will be a difficult task. Translating the objectives into measurable goals depends on the availability of data — and data is often scarce for indicators that cannot be very well defined, for example ‘burden of disease’ (mission 1) or ‘quality of life’ (mission 4). Measuring the inputs, activities, outputs and impacts, as well as causal relationships between them, must be prioritised. Second, to ensure that the quadruple helix is used to the fullest extent, the governance and funding structures of the PPPs must be re-evaluated so that both risks and rewards are shared by public and private actors. In doing so, Health~Holland can ensure that relationships are symbiotic, mutualistic and, importantly, optimise public value for citizens.
 Close
Close

