GADSA - A Gamified Antimicrobial Stewardship (AMS) Decision Support App
A Gamified Antimicrobial Stewardship (AMS) Decision Support App to Encourage Prescribing Behaviour Change in Nigeria

7 February 2019
The Challenge for the Research
Many deaths caused by infectious diseases in lower-income countries could be avoided by better infection prevention and control practices including appropriate prescribing of antibiotics. Inadequate knowledge of infection control and prudent prescribing practice, poor infrastructure, inadequate funding of health care, and staff shortages are all factors contributing to the spread of Antimicrobial Resistance (AMR); a grave global concern threatening the effective prevention and treatment of disease and infections.
Good Antimicrobial Stewardship (AMS) means effective use of antibiotics including compliance with published guidance, reduced instances of inappropriate prescription, dosage, duration and use of broad-spectrum antibiotics. Significant investment has been made in high-income countries (HICs) to understand poor AMS but response to AMR in LMICs, particularly in African countries, has been much slower. At present there is no coherent antimicrobial stewardship framework and training programme in Africa. Just 4% of LMICs have national AMR plans in place and only 15% have national IP&C policies. As high as 20-50% of antimicrobial use in Africa is thought to be inappropriate however it is not yet fully understood why this figure is so high.
Overall Aim
To improve antibiotic stewardship amongst surgeons in Nigeria through sustained behaviour change by developing a persuasive mobile gamified decision support app.
Working with Nigeria

In Nigeria, differences in AMS implementation across multiple settings and the prevalence of a range of medical conditions is essential for assessing the needs of patients. For the GADSA (Gamified Antimicrobial Stewardship Mobile Decision Support App) project, we are working together with colleagues at ICAN and in partnership with surgical teams at the Lagos University Teaching Hospital and Lagos State University College of Medicine.
Background Context

Amongst medical teams, evidence-based guidance is considered necessary yet difficult to tailor to individual patient needs. Some research suggests that inappropriate prescribing decisions by clinicians are driven by complacency, fear of disease progression and fear of losing patients to competitors if no prescription is given. Inappropriate prescribing has been shown to increase with time since qualification with a culture of ‘prescribing etiquette’ meaning that behaviour and habits of senior clinicians can heavily influence the habits of junior staff. The most prominent factors driving poor AMS are, inadequate knowledge of AMR amongst clinicians and patients and poor access to continuing medical education and decision support tools for prescribing professionals. Education for frontline healthcare workers must be significantly improved to translate theoretical knowledge into IP&C practice.
Mobile Decision Support

With over a third of the global population predicted to own a smartphone and internet user penetration projected to grow from 46.8% to 53.7% by 2021, LMICs are increasing their investment in smartphone- based mHealth technology. Research has shown that the use of apps is considered by clinicians as a ‘good idea’ and as an effective way to educate and to improve confidence in compliant prescribing. In high-income countries, apps have shown promising results in improving AMS practice but are rarely informed by behaviour change theory and have struggled to provide solutions that optimally educate and engage the user.
Behaviour Change
Theoretical models of behaviour and behaviour change can help to explain the psychological and structural processes underpinning behaviour and represent an accumulation of the knowledge about mechanisms of action (i.e., how behaviour and behaviour change occurs) and the moderators of change. They are extremely relevant therefore to investigating implementation problems (e.g. poor understanding of, and compliance with prescribing guidance) and to designing implementation interventions (e.g. solutions for improving AMS). Without first understanding how or why poor AMS occurs, we cannot develop effective interventions to improve it. Behaviour change theory has so far played a small role in understanding AMS in Africa.
Serious Games for Health
Game-based mobile tools have potential to improve engagement with text-based guidance and develop theoretical knowledge and practical skills. Serious games and simulations engage the user via a form of organised play and have a proven record of efficacy in helping healthcare workers translate theoretical knowledge and develop new skills into practice. Game-based apps, underpinned by behaviour change theory and integrating the latest evidence on best-practice as quickly as possible, offer a powerful solution for delivery of support and training.
Understanding Current Practice
In the first phase of the GADSA project, we sought to better understand barriers to surgeons’ compliance with published prescribing guidance. We focused specifically on appropriate prescription of Surgical Antibiotic Prophylaxis (SAP) for prevention of Surgical Site Infection (SSI) when preparing for elective procedures.
Using Behaviour Change Theory (e.g. Theoretical Domains Framework, COM-B model) we developed an online questionnaire targeting: (1) the physical or psychological capability of individuals to engage in the target behaviour (e.g. knowledge and skills), (2) the physical or social opportunity (e.g. time, financial resources, social support), (3) automatic or reflective motivation. Questionnaire data was collected from surgeons working at both hospital sites.
Development of the GADSA App
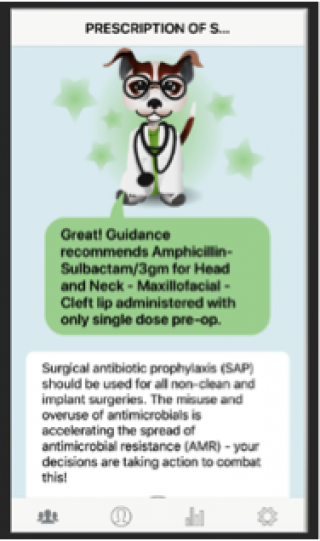
A series of co-design focus groups attended by surgeons at both sites informed selection of evidence-based behaviour change components and gamification features for inclusion in the GADSA app (e.g. a ‘mentor’ providing positive/negative feedback on user decisions to reinforce learning, analytics page showing user performance over time to encourage reflection and self-improvement).
Pilot Test & Evaluation
Following further refinement and input from expert partners both in Nigeria and in the UK, evaluation of a pilot version of the app is scheduled for February 2019. The pilot phase will involve surgeons using the GADSA app during their everyday practice for an 8-week period. The app will collect prescription decisions for approximately 50 surgeons per site. Data collected will be linked to pharmacy databases held at each site and will be analysed for changes in compliant prescribing over time (e.g. prescription of recommended SAPs, appropriate prescription for procedure and patient risk level, avoiding prolonged SAP prescription).
Future Work
We are exploring opportunities to work with other sites across Africa including a third hospital in Nigeria’s Delta State. The decision-based algorithms underpinning the app can be customised for different contexts and to incorporate local policies / guidelines and so we are currently negotiating expansion of the developed technology more broadly across wider Africa, other countries and in different contexts.
Project Funders and Investigators
The Economic and Social Research Council (ESRC). Project reference: ES/P004733/1.
Principal Investigator:
Dr Patty Kostkova, UCL Institute for Risk and Disaster Reduction
Co-Investigators:
Andrei Boscor, UCL Institute for Risk and Disaster Reduction
Prof Andrew Hayward, UCL Epidemiology and Public Health
Dr Carmen Lefevre-Lewis, UCL Centre for Behaviour Change
Prof Sade Ogunsola, University of Lagos, Nigeria
Dr Laura Shallcross, UCL Institute of Health Informatics
Dr Delphine Soriano, UCL Institute for Risk and Disaster Reduction
Dr Caroline Wood, UCL Institute for Risk and Disaster Reduction
Partners:
Dr Andreea Molnar, Swinburne University of Technology Australia
Dr Funmi Bammeke, University of Lagos, Nigeria
Dr Jumoke Olufemi, University of Lagos, Nigeria
Fortune Ncube, ICAN and Public Health England
Sue Wiseman, International Resource for Infection Control
Period of Award
January 2017 – October 2019
Research Programme
GCRF
 Close
Close

