Novel tool counts T cells quickly helping predict patient response to cancer therapy
8 September 2021
Scientists at UCL and the Francis Crick Institute, London, have developed a new tool, which can rapidly estimate the number of T cells (immune cells) in a cancerous tumour*; to help predict a patient’s response to immunotherapy.
Researchers are hopeful that the new findings could enable more targeted and effective cancer therapies.
As part of the Cancer Research UK-funded TRACERx project, published in Nature, scientists analysed DNA sequencing data from patients’ cancerous tumours, to see if they could quantify the fraction of T cells within a sample.
Explaining the research, corresponding author Dr Nicholas McGranahan (UCL Cancer Institute), said: “DNA sequencing is frequently performed on cancer patient’s tumours for patient stratification and to understand how a cancer has developed.
“Estimation of immune cells, which are important for controlling cancers, influencing patient survival and guiding treatment, has in the past not been possible to estimate solely from DNA sequencing data.
“We aimed to explore whether we could develop a novel method to elucidate immune cells directly from DNA sequencing, without the need for more data.”
DNA sequencing allows scientists to see the evolutionary history of how individual tumours have developed. In this research they developed a tool (or method) to ‘look back’ and calculate levels of T cell ‘VDJ recombination’; this is a process in T cells**, in which they are reassembled or altered and given the tools, allowing them to identify and attack invaders.
Specifically, they found a ‘signal’, which indicated the loss of T cell receptor excision circles (TRECs), needed for T cell maturation, which occurred during VDJ recombination. By giving this ‘loss’ a score, they were able to estimate accurately the number of T cells present in the tumour.
Dr McGranahan added: “We show that this score can be used to predict response to immunotherapy and immune evasion mechanisms.
“The score can also be applied to DNA sequencing data derived from normal blood samples that are typically collected but until now have not been able to be systematically analysed for immune content.”
Why this will help immunotherapy
In recent years checkpoint inhibitors (CPIs), a type of immunotherapy, have emerged
as a revolutionary treatment for many cancer types.
CPIs work by blocking proteins called checkpoints, that are made by T cells; these checkpoints help keep immune responses from being too strong and sometimes can keep T cells from killing cancer cells. When these checkpoints are blocked, T cells can kill cancer cells better.
One of the biomarkers found which predict the likely success of immunotherapy is the quantity of T cells present. The more T cells available for CPIs to adapt, the more cancer cells can be destroyed.
First author Dr Robert Bentham, Senior Research Fellow (UCL Cancer Institute), said: “Quantifying T cell infiltration directly from DNA sequencing provides greater predictive power of patient response to treatment without the need for additional data.
“Indeed, the process we’ve developed can be done without additional time or cost, beyond standard DNA sequencing.
“Our tool will also enable more research into the immune system, not only in the context of cancer.”
Scientists say, as the tool has only been used in research so far, they will need to develop it further before it can be made available for clinical use.
UCL was assisted in this study by research partners at the Francis Crick Institute, London, and used patient samples from the CRUK-funded TRACERx study, led by Professor Charles Swanton, Group Leader at the Crick and Director of the UCL CRUK Lung Cancer Centre of Excellence.
Funding was received from Wellcome, Cancer Research UK and Rosetrees.
* The tool/method can work on any sequencing data, so could be applied to other conditions, where DNA sequencing is available.
** VDJ recombination also occurs in B cells (in a different gene). This method could be extended to B cells in future.
Links
- Original research published in Nature
- Dr Nicholas McGranahan’s academic profile
- Dr Robert Bentham’s academic profile
- UCL Cancer Institute
- UCL Faculty of Medical Sciences
- Francis Crick Institute
- Cancer Research UK
- TRACERx study
Image
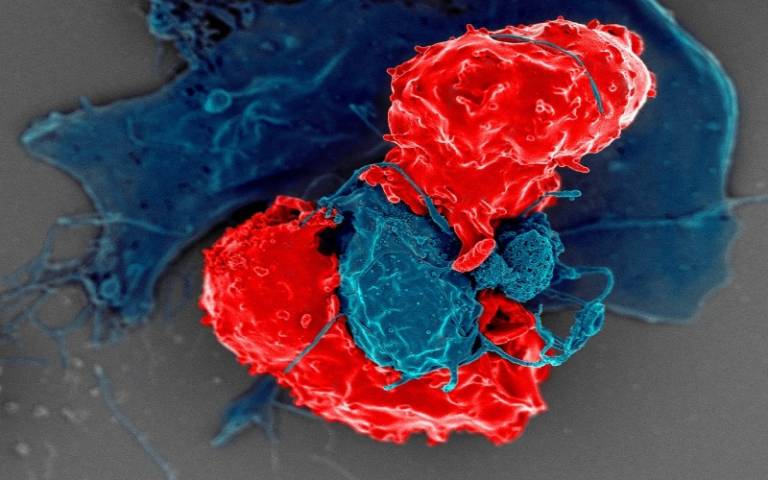
- Electron microscope image of T regulatory cells (red) interacting with antigen-presenting cells (blue). Credit NIAID
Media contacts
Poppy Danby
Email: p.danby [at] ucl.ac.uk
Henry Killworth
Tel: +44 (0) 7881 833274
E: h.killworth [at] ucl.ac.uk
 Close
Close

