Study investigates immune response to Covid-19 in patients with antibody deficiency
11 May 2021
How the immune systems of patients with antibody deficiency respond to SARS-CoV-2 infection and vaccination will be investigated as part of a new national study co-led by UCL researchers.
Funded by UK Research and Innovation (UKRI), ‘COVID infection in patients with Antibody Deficiency’ (COVAD) is part of a portfolio of UK-wide studies examining the immune responses in patients considered at high risk of COVID-19.
Immunodeficiency patients are considered vulnerable or extremely vulnerable to COVID-19 infection and have had to undertake preventative measures to minimise their risk of exposure to the virus.
Patients with antibody deficiency do not make good responses – if any – to most vaccines, but it is not known whether they will respond to COVID-19 vaccines.
The study is being led by the University of Birmingham, University Hospitals Birmingham NHS Foundation Trust, and UCL.
Co-principal Investigator Siobhan Burns, Professor of Translational Immunology at UCL Division of Infection & Immunity said: “This study is part of the national effort to understand how well vaccines work in vulnerable patients. We are also looking for persistent viral infections in our patients to understand whether this drives viral mutation.”
COVAD Chief Investigator Alex Richter, Professor of Clinical Immunology at the University of Birmingham, and Consultant Clinical Immunologist at University Hospitals Birmingham NHS Foundation Trust, said: “Nationally, a number of patients with immunodeficiency have had severe or prolonged illness with COVID-19. Understanding why some patients do well and others don’t is so important. Being unable to clear the virus is not just a problem to the patient but is potentially a public health problem too.”
The researchers will be using Oxford Immunotec’s T-SPOT®.COVID Test* to test immunological responses. Samples will be taken from patients to measure the presence and level of antibodies in the blood and anti-SARS-CoV-2 T-cells.
The results of the research will be widely applicable to immunosuppressed patients and will help inform the development of vaccination strategies as well as strengthen the understanding of risk for continuous virus transmission.
Professor Fiona Watt, Executive Chair of the Medical Research Council, part of UKRI, said: “This multi-partner study will explore a crucial area of COVID-19 research and tell us more about the immune response of immunodeficient individuals to natural COVID-19 infection and vaccination. The importance of this is two-fold: protecting some of the most vulnerable groups to severe effects of the disease, and understanding how the virus that causes COVID-19 may adapt within an individual who struggles to clear the virus.”
Margaret Bennett, West Midlands Patient Representative Immunodeficiency UK, said: “It is important for vulnerable patients with immunodeficiencies to know if the COVID-19 vaccine offers them any protection.”
Professor Sinisa Savic, Chair of the UK Primary Immunodeficiency Network, explained: “The findings of this study will be critical for developing future COVID-19 guidelines for care of patients with antibody deficiencies.”
Dr Andrew Makin, VP of Medical Affairs at Oxford Immunotec, stated: “We are pleased to be partnering with the University of Birmingham on this clinical trial which will help characterize COVID-19 infection in patients with antibody deficiency. Measuring the T cell response in immune deficient patients will allow for a more comprehensive understanding of the immune response and signify the vital role T cells play in SARS-CoV-2 infection.”
Professor Richter and Professor Burns are leading the COVAD research team at immunodeficiency centres at NHS hospital trusts across the UK, in what will be the largest study of its kind in this rare patient group world-wide.
The centres** will screen patients and will invite those who are eligible and meet specific criteria to join the trial. If a patient is eligible for the study, their immunologist will be writing to them with more information. Those who have been written to who wish to take part in the study should call the number provided on their invitation letter, or they should inform the clinical team at their next immunology appointment that they would like to be considered for the COVAD study.
** The immunodeficiency centres are based at the following NHS Trusts: University Hospitals Birmingham NHS Foundation Trust; Oxford University Hospitals NHS Foundation Trust; Salford Royal NHS Foundation Trust; North Bristol NHS Trust; London North West University Healthcare NHS Trust; University Hospital Southampton NHS Foundation Trust; Newcastle upon Tyne Hospitals NHS Foundation Trust; Barts Health NHS Trust; Cambridge University Hospitals NHS Foundation Trust; University Hospitals of North Midlands NHS Foundation Trust; University Hospitals Plymouth NHS Trust; Sandwell and West Birmingham NHS Trust.
Links
- Professor Siobhan Burns' acdemic profile
- UCL Division of Infection & Immunity
- University of Birmingham
- University Hospitals Birmingham NHS Foundation Trust
- UK Research and Innovation (UKRI)
Image
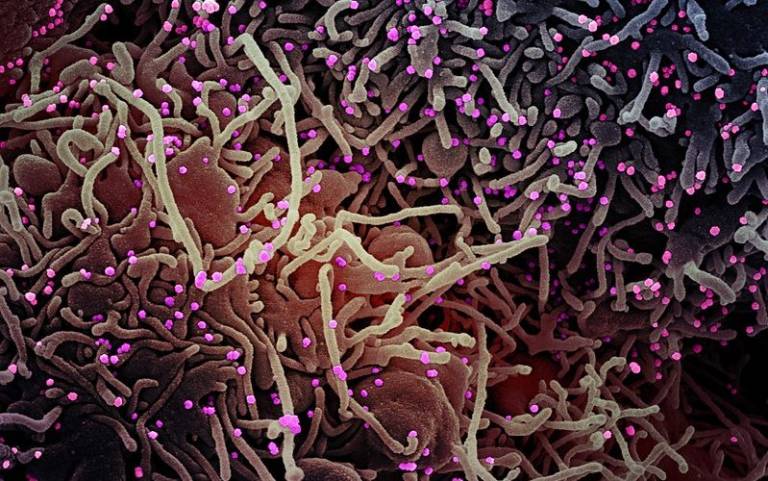
- Colourised scanning electron micrograph of a VERO E6 cell (purple) exhibiting elongated cell projections and signs of apoptosis, after infection with SARS-COV-2 virus particles (pink). Credit: NIAID on Flickr CC BY 2.0
Source
- University of Birmingham
Media contact
Henry Killworth
Tel: +44 (0)7881 833274
 Close
Close

