Prostate cancer ultrasound treatment as effective as surgery or radiotherapy
6 July 2018
Using high energy ultrasound beams to destroy prostate cancer tumours may be as effective as surgery or radiotherapy, but with fewer side effects, a report co-led by UCL has found.
The research, carried out across six UK hospitals, tracked the registration data of 625 men with prostate cancer who received a type of treatment called high-intensity focused ultrasound (HIFU).
The report is the largest ever of HIFU treatment used to target prostate tumours. The treatment is similar to a 'lumpectomy' for other cancers - where doctors remove only tumour cells, leaving as much healthy tissue as possible.
The findings, from a number of institutions including Imperial College London and UCL, found that after five years the cancer survival rate was 100%. Approximately, 1 in 10 men needed further treatment. The cancer survival rate from surgery and radiotherapy is also 100% at five years.
The research also showed the risk of side effects such as urinary incontinence and erectile dysfunction were lower than other treatment options, at 2% and 15% respectively.
The study, published in the journal European Urology, was funded by the Medical Research Council and Sonacare Inc., who manufacture the ultrasound equipment used in the procedure.
Ms Caroline Moore (UCL Surgery & Interventional Sciences), said: "The registry based data from over 600 men is very encouraging. We started the HIFU programme at UCLH in 2003, and now principally use it as a focal treatment, where we treat the cancer but not the entire prostate. This means that men are much more likely to preserve urinary and sexual function, compared to traditional surgery or radiotherapy. Focal treatment is particularly suitable for men who have prostate cancer visible on MRI, which is contained to one area of the prostate."
Prostate cancer is the most common cancer in men in the UK, with around 47,000 cases every year.
Treatments include surgery to remove the gland, or radiotherapy, which uses radiation to the entire prostate.
However, these treatments can cause collateral damage to surrounding sensitive tissues like nerves, muscles, urine passage, bladder and rectum. The prostate is roughly the size of a walnut and sits between the bladder and the penis.
Surgery and radiotherapy to the entire prostate are effective treatments but can lead to long term risk of urinary problems, like incontinence, of between 5-30%. They also carry a risk of erectile dysfunction of between 30-60%. Radiotherapy can also cause rectal problems like bleeding, diarrhoea and discomfort in five per cent of patients.
HIFU is a newer treatment, performed under general anaesthetic, which delivers beams of high energy ultrasound directly into the prostate gland, via a probe inserted up the back passage. There are no needles or cuts to skin. This allows a surgeon to precisely target tumour cells within the gland to millimetre accuracy, with less risk of damage to surrounding tissues.
Professor Hashim Ahmed, lead author from Imperial College London, said: "Although prostate cancer survival rates are now very good, the side effects of surgery or radiotherapy can be life-changing. Some patients are left requiring multiple incontinence pads every day, or with severe erectile dysfunction."
He added: "We need to now focus on improving the quality of life for these men following treatment. This latest trial of focal HIFU - which is the largest and longest study of the treatment to date - suggests we may be able to tackle the cancer with fewer side effects."
In the new HIFU study, conducted on men with an average age of 65 and whose cancer hadn't spread, the risk of urine incontinence (defined as requiring pad use) at five years after the treatment was 2%, and the risk of erectile dysfunction 15%. The team say the results include patients with medium to high risk cancer.
The scientists also tracked the number of patients who needed further treatment following HIFU, (such as surgery or radiotherapy), to treat any cancer cells that had returned. They found 10% of patients needed further treatment by five years, which is comparable to number of patients needing further treatment after surgery or radiotherapy (5-15%).
The team add that prostate cancer patients should talk through all possible treatments with their healthcare team, so they can consider their options fully.
Further follow-up trials are needed to track progress of the patients after ten years, as well as trials that directly compare HIFU with surgery and radiotherapy.
Links
- Research paper in European Urology
- Ms Caroline Moore's academic profile
- UCL Surgery & Interventional Science
- UCL Medical Sciences
Image
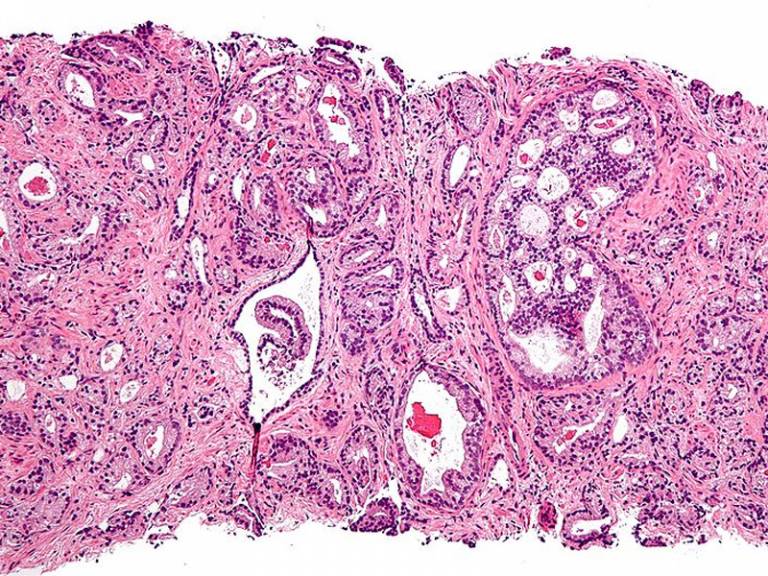
- Micrograph of prostatic adenocarcinoma, the most common form of prostate cancer (Credit: Nephron, Source: Wikimedia Commons)
Source
Media contact
Chris Lane
Email: chris.lane [at] ucl.ac.uk
 Close
Close

