The problem
With Covid looking to stay with us long term, and hospital waiting lists increasing, it is important that we come up with strategies to help keep indoor environments safe. Aerosol particles are droplets generated from expiratory events such as breathing, talking and coughing. They play a critical role in the transmission of infectious respiratory diseases, such as Covid-19. Reducing droplet spread is essential for infection control, particularly in high-risk environments such as hospitals.
The CONFESS study undertook a detailed analysis of droplet concentrations, during different expiratory activities such as breathing, talking, singing and coughing. They found a wide variation between people in terms of the number of droplets they produce for different vocal tasks, however the number and velocity of droplets are dramatically reduced by wearing face masks.
With an increase in anti-mask sentiment, the impracticality of healthcare staff wearing facemasks longterm, and the government taking steps away from compulsory face masks, it seems that we may need alternative solutions.
Potential alternative mitigation strategies include increasing air flow, using air filters and personal ventilation. The Safe Air study aims to investigate the effectiveness of these mitigation strategies to develop key recommendations that can help to safely increase patient flows in hospitals.
How are we investigating?
There are two ways in which the researchers are investigating this problem. The first is by using computer modelling. By building computational models of actual consulting rooms at UCLH, with a patient and doctor present, the researchers are able to see which mitigation strategies have the potential to be the most effective at reducing droplet concentration.
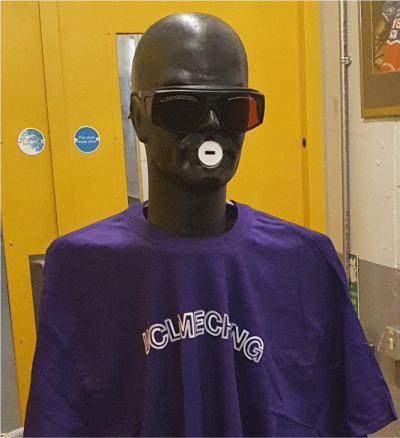
The researchers are also carrying out practical experiments using a robot that they have built called ‘Sonny’ - a virtual human exhalation replicator (VALUATOR). This produces aerosols like humans which means that the team can measure aerosol production in real locations, even measuring the interaction of aerosols from two valuators – simulating a patient doctor interaction.
What have we found so far?
Computer simulations have been carried out with numerous scenarios: air conditioning, a fan, Perspex screens and HEPA filters. It was found that aircon, without any other mitigations in place, was detrimental as it encouraged droplet spread, whereas without aircon the majority of droplets landed on surfaces.
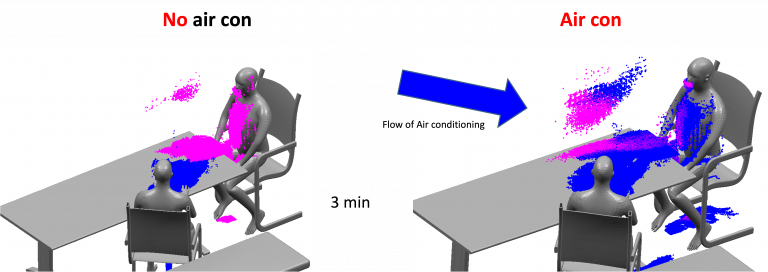
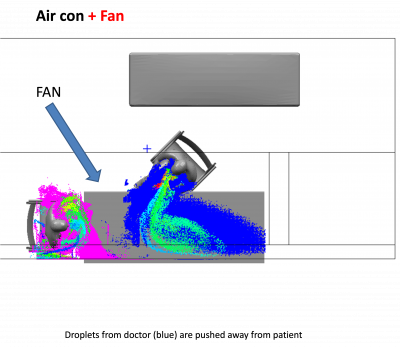
Modelling using a fan showed that this may be a good mitigation strategy, as when placed between a patient and doctor, this pushes the droplets away from each other.
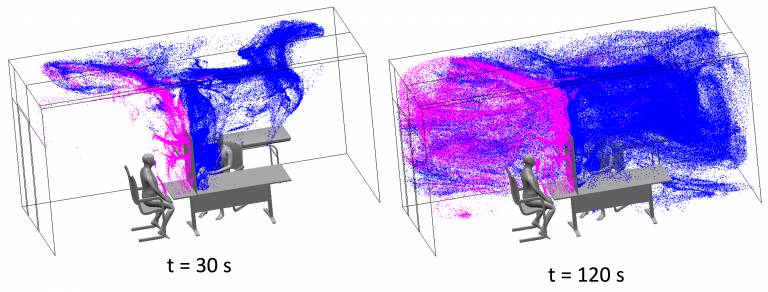
Clear Perspex screens have become a common mitigation strategy during Covid. Simulations demonstrated that while this was effective for very short periods, after 60 seconds there is droplet mixing between the doctor and patient meaning that it is an ineffective mitigation strategy in the long term.
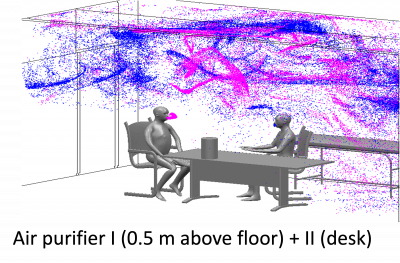
HEPA (High Efficiency Particulate Air) filters are a further potential mitigation strategy. They are relatively cheap to buy, portable, quiet to run, and remove >99.7% of particles larger than 300nm. These filters are effective at reducing droplet spread, however computer modelling shows that the location of the filter is important, with highest effectiveness when the filter is placed 1m above the floor. Further modelling showed that two filters are better than one – with one air purifier on the floor and the second placed on a desk between the doctor and patient.
Using Sonny in a laboratory, the researchers have set up a variety of experiments to measure droplet clearance. In comparison to a room with no ventilation, air con dramatically reduces the peak number of droplets, and the addition of two filters further reduces this peak. With HEPA filters, droplet half-life is also dramatically reduced, showing a clear benefit of air filters as a mitigation strategy.
When these experiments were replicated in real hospital rooms, the results showed an 85% reduction in peak droplet concentration and 92% faster air cleaning when the room was vacated when two air filters were used in comparison to no ventilation.
Overall these experiments illustrated that when two air filters were used in a room with no airflow there was a dramatic reduction in particle build up and a further dramatic reduction in particle clearance. The results of these experiments suggest that rooms that weren’t previously deemed safe can now be used with the use of two retail HEPA filters with a total cost of under £400.
Next steps
The next steps in this study are to start examining the effects of air filters in waiting rooms, in both high- and low-density areas, in seminar rooms, and UCLH wards to prevent patient to patient transmission. As well as this issues to consider are how to roll out the use of HEPA filters across the trust, raising staff awareness and considering the wider impacts such as on schools.
 Close
Close

