Transforming treatment for glaucoma patients and reducing healthcare costs
UCL-led research has demonstrated the clinical- and cost-effectiveness of selective laser trabeculoplasty (SLT) for glaucoma, leading to changes to clinical guidelines in the UK, Europe and the US.
28 April 2022
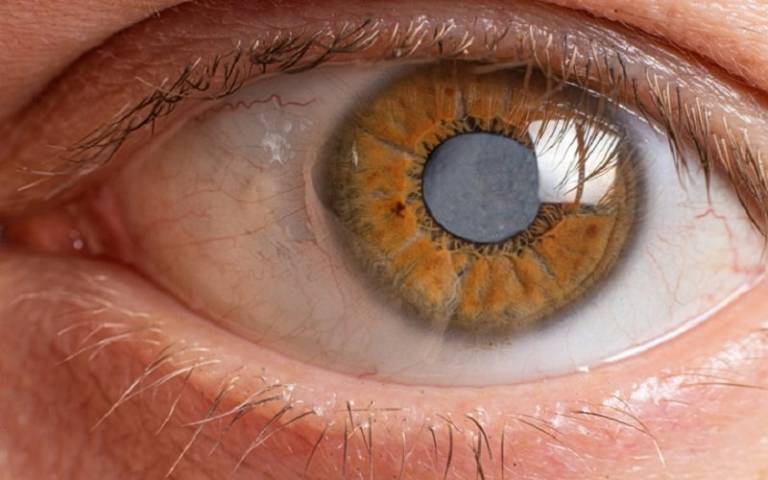
Glaucoma affects approximately 76 million people worldwide including over half a million people in the UK, where it is a leading cause of visual morbidity. It is caused by progressive damage to the optic nerve resulting from raised pressure inside the eye (Intraocular Pressure, or IOP). Ocular hypertension (OHT), a state of raised IOP in otherwise healthy eyes, is a risk factor for developing glaucoma that affects 1.2 million individuals in the UK.
In the UK alone, there were more than a million glaucoma-related hospital visits in 2012 and eight million glaucoma treatment prescriptions dispensed in the community, costing the health service over £105 million.
The traditional first-line treatment for glaucoma and OHT is IOP-lowering eyedrops, which can have side effects that impact quality of life. These side effects include those affecting the eye, such as burning or stinging, and those affecting the entire body such as a decrease in blood pressure. A third of patients prescribed eye drops for glaucoma stop collecting their prescriptions within the first year, due to difficulties in administering them.
A quick and painless alternative to eyedrops
The UCL team’s research found that a quick and painless alternative, administered at an outpatient’s clinic – 360-degree Selective Laser Trabeculoplasty (SLT) – reduces IOP to a similar level as either eyedrops alone, or a combination of drops and surgery.
Professor Gus Gazzard (UCL Institute of Ophthalmology and Moorfields Eye Hospital) led a clinical trial involving over 700 glaucoma patients with open angle glaucoma or OHT across six NHS sites – Laser in Glaucoma and Ocular Hypertension Trial (LiGHT). It demonstrated that patients can be safely treated with SLT and achieve eyedrop-free IOP control over at least three years and a reduced need for glaucoma and cataract surgery, compared to patients treated with routine medical treatment only.
Importantly, this can be achieved at a lower cost per Quality Adjusted Life Year (QALY) than standard medical therapy alone and with a similar effect on general health-related quality of life while better preserving vision. Primary SLT is a cost-effective, repeatable alternative to eyedrops that can be offered to patients with OAG or OHT who need IOP-lowering treatment.
Changing clinical guidelines and reducing costs
In 2020, European and American clinical guidelines were updated to recommend SLT as an initial treatment for IOP and glaucoma. The UK’s NICE guidelines state that SLT is a cost effective first line option for treatment. As of January 2022, NICE now advises SLT be offered to all open angle glaucoma and ocular hypertension patients.
As a result of the uptake of SLT, the cost savings in ophthalmology services in England alone are estimated to have been as much as £524million.
One patient who has undergone SLT is Guy Staniforth, 62, a project engineer from Greenwich in South-East London. He said of the experience:
I was pleased to be told I’d be having laser treatment, as taking daily drops would be a nuisance. I didn’t feel a thing, but straight afterwards my eye pressure had fallen from 28mmHg to 14mmHg – ‘normal’ is less than 22mmHg. I had no side-effects and was told to carry on as normal. I so appreciate what’s been done for me at Moorfields. I really hope it can help others with glaucoma as it has me.
YouTube Widget Placeholderhttps://www.youtube.com/watch?v=cR2NC6iQNIw
Research synopsis
Transforming clinical practice and achieving significant cost savings in the treatment of glaucoma
Research led by UCL has demonstrated the clinical- and cost-effectiveness of selective laser trabeculoplasty (SLT) over daily eyedrops and surgery to reduce internal eye pressure in people with glaucoma. The findings have transformed treatment for glaucoma through changes to clinical guidelines in the UK, Europe and the US, reducing outpatient appointments and costs.
Links
- Professor Gus Gazzard’s academic profile
- UCL Institute of Ophthalmology
- Moorfields Eye Hospital NHS Foundation Trust
- UCL Faculty of Brain Sciences
- UCL Faculty of Brain Sciences - REF 2021
- Transforming clinical practice and achieving significant cost savings in the treatment of glaucoma video
Image
- Image credit: istock / Zarina Lukash
 Close
Close

