Healthcare Engineering & Ethnic Inequalities Event
24 April 2023
On 23 April 2023, we held a panel event, ‘Healthcare Engineering and Ethnic Inequalities’, to explore the issue of ethnic inequality in healthcare engineering and medical devices and learn how engineers can improve the situation. Here's the issues and solutions discussed.
We know there’s a problem: racism. Unfortunately, racism is also an issue in the world of healthcare engineering with Covid-19 really highlighting the problems a lot of the global majority are facing.
On 23 April 2023, we held a panel event, ‘Healthcare Engineering and Ethnic Inequalities’, to explore the issue of ethnic inequality in healthcare engineering and medical devices and learn how engineers can improve the situation.
The IHE’s Deputy Director of Translation, Geoff Parker, introduced the event with a few words on why this matters and why it’s important we tackle healthcare inequalities – mainly to ensure people do not face unequal outcomes, to the extent of death, because of implicit biases within our healthcare system.
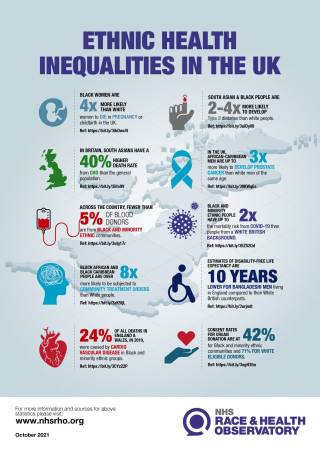
Dr. Shoba Poduval, GP and NIHR academic clinical lecturer at UC, was our first guest. She started off by talking about her research which shows that interventions are needed on all levels, especially when it comes to data science and machine learning, sensors and wearables and diagnostics. This ties in with the government’s own call for evidence ‘from those who work closely with medical devices such oxygen measuring devices and infrared scanners and other medical software and hardware, including databases and instructions for medical devices.’ [Source]
In machine learning, a lot of the data is from white, heterosexual men which is a problem when creating tools and devices for everyone, especially those with darker skin tones. The problem of data also raises the issue of data collection and how, on top of data not reflecting the British communities we have here, there isn’t data transparency. Healthcare professionals need to tell their patients why they’re collecting data plus how it is being used so patients are involved and can see how they too are helping the cause.
But how can we solve this issue of data? Dr. Poduval suggests more Digital Health Hubs which are community organisations designed to help people who are socially and digitally excluded so they can access the tools and devices to help their wellbeing. She also suggests colocation spaces, peer support and finding ways to help people navigate online and physical spaces.
There also needs to be more inclusive research practices which can help address the under representation of ethnic minorities in research. Dr. Poduval suggests we need to work with these communities not just by giving out flyers but by being in the spaces people are comfortable in.
Shoba covered a lot of ground and our next speaker, Laura Katus was here to add to the event by sharing her experience of working in neurodevelopment within the context of poverty-related risk in a cohort in rural Gambia. Professor Laura Katus is a lecturer in psychology at the University of Greenwhich. In her research, she found challenges such as braids not allowing the device she was using to be attached properly to children's heads, or the climate the humid climate eroding electronics. But these weren’t issues to stop her research. By understanding the culture, Professor Laura and her team were able to find solutions like hiring a professional hairdresser to re-braid hair.
The team also found unfamiliar environments and interactions with unknown staff naturally made children more reserved, so it was key to create stimuli that was culturally appropriate, and that the children were familiar with – which is what they did. They hired workers from the community to help the children feel at ease and create an environment they were comfortable with.

Lastly, we had Patience Renias-Zuva who is the PPI Manager at the UCLH BRC and looks at ways to involve the public in research. One of the things she mentioned is that researchers can include people from the get-go! But you should be held accountable by your patients by including them in the findings – which is what Professor Poduval also mentioned. A lot of the time, patients don't know why their data is being collected and this builds distrust. A prime example used was no reason given as to why ethnicity being asked for during Covid-19 vaccinations.
Patience also mentions that when applying for grants, make sure you have solid reasoning why you need patient input and how the patient fits into your application eg. are they a coproducer, PPI etc.
If you are interested in working with the public for your healthcare research, then please get in touch with Patience by contacting her at ppihelpdesk@ucl.ac.uk
During the panel discussion, language was covered. Global south/north? BAME? Global majority? There's problems with all terms but the government has realised that BAME was one that should be dropped. Whilst negative language like 'hard to reach communities' and time constraints hinder accessing communities whose input is key in making research more relevant to the people it’s looking to serve.
Through this all, we’ve realised that we don’t have enough healthcare engineers working to eradicate the problems being faced by the global majority. If you’re interested in tackling the issues faced then please get in touch with us.
 Close
Close

