PHOTONIC: analysing the implementation and impact of prehospital video triage for suspected stroke.

Stroke is a major cause of death and disability in the UK and worldwide. Stroke patients get better care and have better outcomes if treated in a stroke specialist unit, but currently such units also treat many patients who have not had a stroke.
During the COVID19 pandemic, some parts of England introduced prehospital triage interventions that let hospital-based stroke specialists use digital videoconferencing to communicate remotely with ambulance clinicians to assess suspected stroke patients. These aim to ensure patients are taken to the right service (or stay home, if appropriate). However, little is known about implementing these interventions in different settings, how well they work, their impact on care and outcomes, and whether they provide value for money.
PHOTONIC (PreHOspital Triage for potential stroke patients: lessONs from systems Implemented in response to COVID19) builds on our recent rapid service evaluation of prehospital triage in North Central London and East Kent, which focused on safety, effectiveness, and usability (Link).
Our team (details below) includes stroke survivors, stroke and ambulance clinicians and service managers, charities, and researchers. We will study four areas, NC London, East Kent, Maidstone, and Darent Valley, which have recently implemented prehospital triage.
Our research questions
1. Which factors influence implementation, use, and expansion of prehospital triage for suspected stroke patients, in terms of planning, governance, and workforce?
2. How is prehospital triage experienced by patients and carers (of different backgrounds), stroke and ambulance services, emergency departments, primary care, TIA clinics, hospital managers, system leaders, and charities?
3. Does prehospital triage impact on ‘appropriate’ patient transfer, care delivery, and patient outcomes across the prehospital and acute stroke pathways?
4. Is prehospital triage for stroke cost-effective?
5. What are the lessons for planning, implementing, and evaluating prehospital triage (for stroke and other conditions)?
Our approach
Here is a short video that explains what PHONOTIC is about:
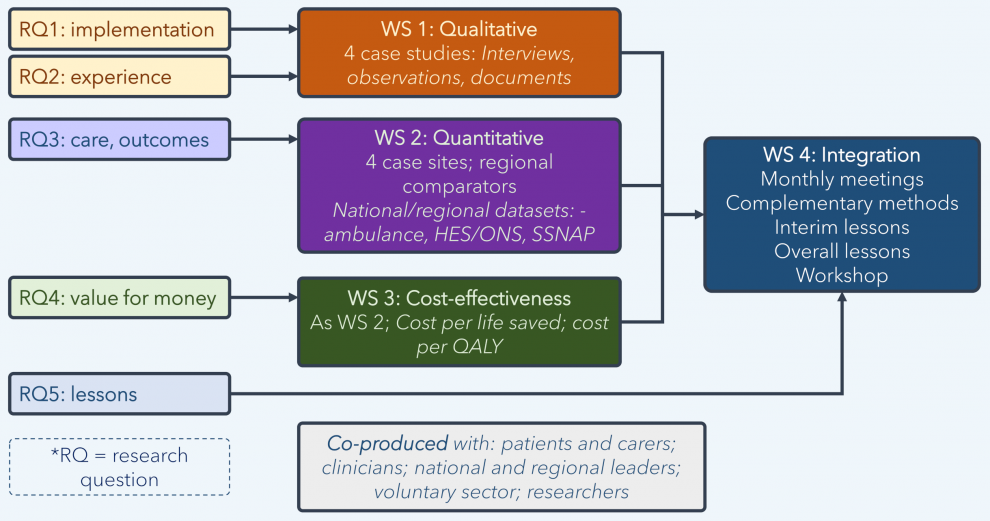
Qualitative research to understand implementation and experience of services
First, we will study how prehospital triage is set up, run, and experienced. We will interview patients and carers; stroke, ambulance, and emergency teams; and service and system managers. We will observe oversight and delivery of prehospital triage and study relevant documents. We will ask how the services were put into action, and what helped or hindered this. We will also ask patients and carers how they experienced prehospital triage.
Understanding impact on care delivery, outcomes, and cost-effectiveness
Second, we will use NHS data to study the impact of prehospital triage on healthcare services (e.g. ambulance journeys and stroke care delivery), patient outcomes (e.g. patient mortality), and value for money. We will analyse performance before and after prehospital triage was introduced, comparing the areas that are using prehospital triage with other parts of the UK that are not.
Integration of findings
Our mixed-method approach will let us combine our findings to identify common themes across participating services and points of contrast between them. We will use our qualitative data to explain quantitative and cost-effectiveness finding, and to examine issues not available through quantitative data.
Sharing learning
Our study will provide important lessons on how prehospital triage for stroke affects quality of care, patient outcomes, and value for money. Throughout, we will engage with the people leading prehospital triage in monthly meetings, so they can make use of our findings as they develop. We will develop a list of clinicians, politicians, charities, members of the public, and others who make decisions about healthcare and are interested in our research; we will share with them quarterly newsletters and podcasts to describe how our research is going. When we are sure of our findings, we will present them at research conferences and in academic journals, and make accessible summaries and podcasts for stakeholders. Finally, we will run a workshop for people providing stroke and other services, patients and carers, charities, and international experts, to share and develop lessons for services across the UK that might want to introduce prehospital triage.
Start date and duration:
September 2021 – June 2024
Funder:
National Institute for Health and Care Research (NIHR) Health and Social Care Delivery Research programme (Ref: NIHR 133779)
Amount Awarded:
£592,411.19
 Close
Close

