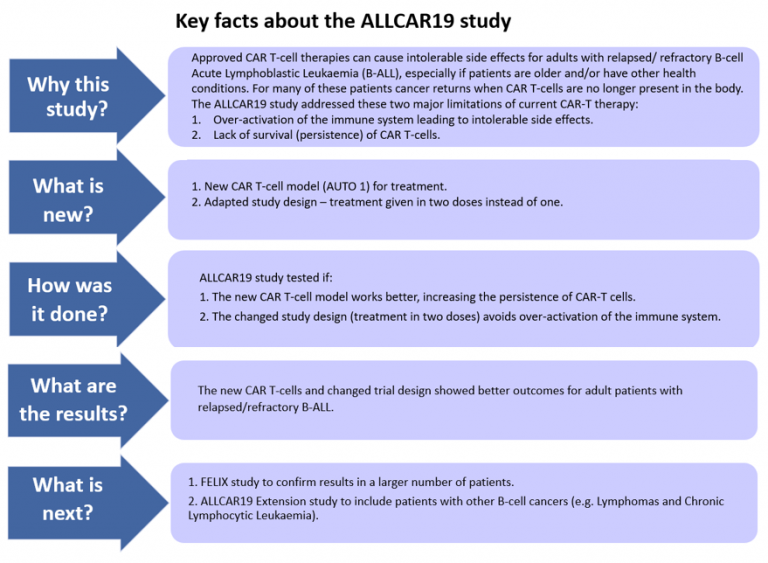
New CAR T-cell therapy ALLCAR19 for adults with relapsed/refractory B-cell Acute Lymphoblasic Leukaemia shows promise as stand-alone treatment
This plain English summary explains challenges of CAR T-cell therapy addressed in the ALLCAR19 first-in-human clinical study for adults with B-cell Acute Lymphoblastic Leukaemia (B-ALL), study results and next steps.
“While CAR T therapy is very effective for some patients, current CAR T-cell treatments have limitations. In the ALLCAR19 study we addressed two main problems of CAR-T therapy in adults with relapsed B-cell Acute Lymphoblastic Leukaemia as there is no licensed treatment in this age group for this type of cancer.
Professor Karl Peggs, Chief Investigator of the ALLCAR19 study and Co-Director of the Blood and Transplant Research Unit in Stem Cells and Immunotherapies at UCL
“As both scientists and doctors, we are delighted with the results; they are important because they show the new CD19 CAR design allows for the safe treatment of CAR T-Cell therapy to adult patients with relapsed B-ALL. Moreover, this treatment may allow patients to have long-term remissions with no other treatment.
Dr Claire Roddie, Associate Professor at UCL Cancer Institute, consultant haematologist at UCLH and Director of the Blood and Transplant Research Unit in Stem Cells and Immunotherapies at UCL
Read the full
Questionnaire about views on communicating early clinical cancer studies
Following feedback on the documentary 'War in the Blood' we launched a questionnaire to learn about the impact of the documentary and ways to communicate cancer studies. Many thanks to all respondents for taking the time to complete this questionnaire, and to members of the Patient and Public Research Panel at the BTRU in Stem Cells and Immunotherapies at UCL for shaping the questionnnaire. View the report of replies on the questionnaire about views on communicating early clinical cancer studies
Improving Patient Information Sheets: Learnings from a workshop with cancer trial managers and patient and public partners
Ten BTRU Patient and Public Research Panel members worked with twenty-four Trial Managers from the Cancer Research UK UCL Cancer Trials Centre to improve Patient Information Sheets (key documents for making informed decisions to participate in clinical studies). Read about the workshop and top tips to make Patient Information Sheets easier to read and understand in this blog post.
Research communication: Involve patients and carers in the conversation
In our recent blog post we wrote with patients, cares and advocates about the benefits of communicating research and top tips on how to do this successfully.
The blog is based on a recent conversation between clinicians, lab-based researchers, the Sickle Cell Society and people affected by sickle cell disorder that clearly showed the need for better communication and the importance of including views of patients early on in health care research. While it specifically look at research into sickle cell disorder, other patient groups may share similar views in regards to patient involvement, and therefore the perspectives shared are a helpful starting point for all translational research.

Image credit: Canva
New CAR T-cell therapy offers hope for blood cancer patients
Read about recent research of our BTRU Directors Claire Roddie and Karl Peggs developing new treatments for blood cancers in UCL Hospitals (UCLH) Magazine Issue 16, 2022
New treatment has fewer ‘toxic’ side effects and may target and kill cancer cells for longer, a study at UCLH has found. This offers new hope to adult patients with relapsed B-cell acute lymphoblastic leukaemia for which there is currently no approved curative therapy available. Patients typically have further chemotherapy and the prognosis is poor.
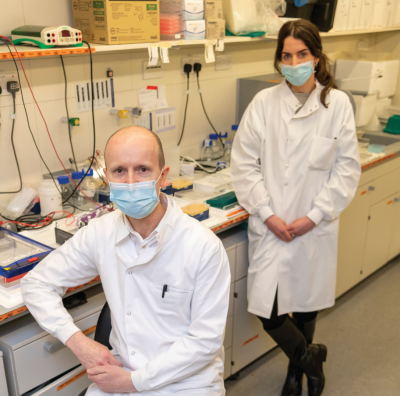
Image description: Professor Karl Peggs and Dr Claire Roddie
- Second generation of CAR T-cell therapy trialled in patients, a NIHR UCLH Biomedical Research Centre (BRC) article from 7 January 2022
- Patients benefit from revolutionary cancer treatment, BBC News from 7 January 2022
New CAR T-cell therapy treatment on BBC News at ten on 7 January 2022 (starting at minute 24:03)
Early research on a gene therapy to treat Sickle Cell Disease
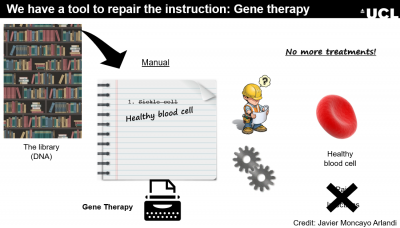
Image credit: Javier Moncayo Arlandi
On 2 September 2021, we hosted an online conversation to hear what it is like to live with Sickle Cell Disease and to talk about three potential future treatments for Sickle Cell Disease with a group of people living with or caring for someone with this condition. The event was hosted with the Sickle Cell Society and fully booked in less than a week. It included a researcher from Theme 2 in our unit, who talked about his work on a potential gene therapy, and a member of our Patient and Public Research Panel among other speakers. Read the full summary
“‘Thank you everyone, this was so helpful and impactful.’ 'As I expected, the session was very informative and such a positive experience. (…), it was empowering to get information and share knowledge.’
Watch the BBC Two documentary ‘War in the Blood’ about CAR-T therapy now on vimeo

The documentary portraits scientists, doctors, and first and foremost two patients and their families taking part in early CAR-T cell therapy studies. It is thanks to their bravery that CAR-T therapy is available as an NHS treatment for some blood cancers today. Watch on Vimeo
“Absolutely fantastic documentary. I was so overwhelmed with emotions watching this, as I have just gone through CAR-T cell therapy myself under Claire Roddie also. In clinic appointments they talk about the trials and patients that have come before you, which inevitably turn into another statistic in your head, so to be able to put a face to these brave and courageous individuals that have paved the way for research and development in this line of treatment means a great deal to me. Thank you for making such an outstanding film that is raising awareness for CAR-T cell therapy.
Insights on including Patient and Public Involvement (PPI) in Advanced Therapies
Hear insights on how Patient and Public Involvement (PPI) improves the quality, strength and relevance of advanced therapies (new medical treatments that use tissue engineering, cell and gene therapy) from our recent Therapeutic Innovation Networks (TINs) seminar jointly hosted with the Cell & Gene Therapy and Regenerative Medicine TIN.
The seminar welcomed the varied perspectives of leading researchers, clinicians and patients, outlining the importance of patient perspectives in research to optimise the real-world impact.
I’m a big believer that we should start to think about PPI early in the translational process, and not wait until it’s too late to engage. - Dr Nick Hamiliton, Ear, Nose,Throat (ENT) surgon and NIHR Clinical Lecturer at UCL
Co-developing training for researchers with patients and members of the public
Read this blog post about our Patient & Public Research Panel members helping to develop a training resource for translational researchers about stakeholder engagement. Anna voices why being involved in research early matters to her as a patient and how much her experience can add to translational research.
Launch: Animation explaining Gene Therapy

Young people asking questions about gene therapy in the animation 'Gene Therapy explained: Chaning out bodies' recipe to treat disease'
21 Januray 2021 - Join us to explore a potential new treatment, called gene therapy. Gene therapy helps to treat some inherited diseases passed on from parent to child that don’t have a treatment or cure yet. Many different gene therapies are currently in development all over the world for inherited diseases such as those that affect the ability of our blood’s immune system to fight off infections.
The animation shows, Alexis and Freddie, two members of the Young Persons’ Advisory Group (YPAG) at Great Ormond Street Hospital for Children asking questions to understand what gene therapy is about. All members of the group were involved in shaping the animation and they regularly work with doctors, nurses and scientists helping to improve health care research for children.
I spent most of my career as a researcher developing gene therapies for children who have an immune system that doesn’t function properly. The immune system of these children can’t protect them from infections and they can become life-threatening. A lot is said on the news about gene editing, less how it can help to treat inherited diseases. Alexis and Freddie helped us to brilliantly explain just this in our animation. We hope it finds much interest and explains a ground-breaking future treatment for some inherited conditions. - Adrian Thrasher, Professor in Paediatric Immunology and Research Lead at the NIHR Blood and Transplant Research Unit in Stem Cells and Immunotherapies at UCL
Watch this brand-new animation ‘Gene Therapy explained: Changing our bodies’ recipe to treat disease’ and read more in our blog post.
Research summary: Editing DNA to produce universal T cell therapies
by Roland Preece, former PhD student in Research Theme 4
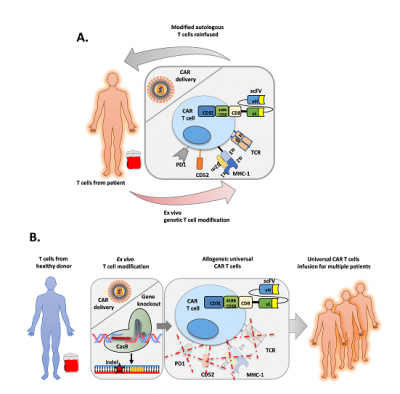
Image credit: Roland Preece
1 December 2020 - T cells are a group of white blood cells that make up an essential component of the immune system, protecting the body from bacterial and viral infections, and preventing the formation of cancers. An emerging branch of therapies referred to as T cell immunotherapies aim to harness the power of these important immune responses and redirect them towards cancer cells while avoiding the damage of healthy tissue often associated with chemotherapy. Such therapies have proven particularly successful against cancers like B cell acute lymphoblastic leukaemia (B-ALL) which uses the patient’s own T cells engineered in a laboratory to recognise a marker only found on B cells (CD19).
T cell immunotherapies have to be made with the patient’s own white blood cells to prevent the treatment from turning on the body of the patient and causing graft versus host disease (donated cells attacking the recipient’s body). The need to produce these therapies for each individual patient limits the wide-spread availability of this therapy as 1) it requires a centre with the expertise to make them and 2) the relatively long time to produce the therapy (~2 weeks) is not be suitable for all patients.
Read the full summary:
Successful 18-months funding extension for BTRU research

Image credit: Pixabay
25 May 2020 - We are delighted to announce a successful 18-months funding extension for our unit at UCL and three other Blood and Transplant Research Units (BTRUs) at University of Cambridge, Newcastle and Bristol. The National Institute for Health and Care Research (NIHR) has extended funding for research at all BTRUs until 31 March 2022.
Working with the UCL BTRU Lay Panel on ways to integrate Patient and Public Involvement in the proposed research was very rewarding and led to some novel ideas to add real value to our programme. – Professor Karl Peggs, former Director and now Co-Director of the UCL BTRU
Read more about Patient and Public Involvement in funding applications in our blog post 'How to get millions in support of your funding bid'.
Cancelled: Hands-on activities for families about CAR T-cell therapy at Cambridge Science Festival 2020
11 March 2020 update: Sadly, the Cambridge Science Festival has been cancelled due to COVID-19.
Visit us at the Cambridge Science Festival: BTRU researchers working on CAR T-cell therapy and Lay Panel members are running hands-on activities about CAR T-cell therapy at the Cambridge Academy for Science and Technology (Robinson Way, Cambridge CB2 0SZ) on Sunday 22 March 2020, 11am - 4pm. The event is free to attend, no booking needed.
Meet our team and two other BTRUs to explore ongoing research to find better and new treatments for people with blood disorders, such as blood cancer, and for patients in need of blood and organ transplants.
For more information visit https://www.sciencefestival.cam.ac.uk/events/t-cell-attack
Broadcast again: 'War in the Blood' documentary about CAR T-cell therapy

Image credit: BBC Two
The BBC Two documentary 'War in the Blood' following two patients through groundbreaking 'first in-human' trials for CAR T-cell therapy to treat blood cancer is broadcasted again on Monday 20 January 2020 at 9pm on BBC Two
How to get millions in support of your funding bid

Involving patients and carers brings the lived experience to medical research. Credit: iStock.com/FatCamera
You may be thinking £’s, $’s or even €’s? We’re thinking people – although one may very well lead to the other.
Read in a blog post of the UCL Translational Reserach Office how we integrate Patient and Public Involvement in proposed research at the NIHR Blood and Transplant Research Unit at UCL, leading to novel ideas and added value.
#MadeAtUCL - Using our own immune cells to target and kill cancer

Image credit: UCL
#MadeAtUCL is showcasing the top 100 stories of disruptive discoveries from UCL. One of them are CAR T-cell therapies, groundbreaking cancer treatments which reprogramme the patient’s own immune system to recognise and kill cancerous cells. Read on
Europe’s first dedicated cellular immunotherapy unit at UCL Hospital
Professor Karl Peggs (former Director and now Co-Director of the NIHR BTRU at UCL) will lead the Sir Naim Dangoor Centre for Cellular Immunotherapy an eight bedded unit at UCL Hospital (UCLH) within the new surgery and cancer building, due to open in 2020. The research and treatment Centre will build upon the world renowned expertise and ground-breaking advances already made at UCLH to successfully treat cancer using cellular immunotherapy. This involves taking live cells from the body and genetically engeneering them to kill cancer cells before re-infusing them to the patient.
The establishment of this Centre will enable UCLH to focus research on advancing cellular immunotherapies. As Professor Peggs says
While clinical translation of cellular immunotherapy research into blood cancers has already shown positive outcomes, more research is desperately needed. We anticipate that through this research, treatment for other types of cancer – such as skin, ovarian, liver and lung cancers – will be developed, meaning greater cancer survival rates. It is a very exciting development that could be a game changer for the treatment of cancer.
'War in the Blood' a documentary about CAR T-cell therapy

'War in the Blood' on BBC iPlayer, image credit: BBC TWO
A new BBC film looks at the work of scientists at UCL and clinicians at UCLH working together on groundbreaking ‘first in-human’ immunotherapy trials.
It is an intimate, feature-length documentary following two patients through groundbreaking ‘first in-human’ trials for CAR T-cell therapy, a treatment described as the beginning of the end of cancer.
Not allowed to meet and separated by two floors of a hospital, 53-year-old Graham and 18-year old-Mahmoud are nevertheless bound together by their commitment to the treatment and their faith in the science. Terminally ill, the trial represents their only option. How do their ages and life experiences affect their physical and emotional response?
Find out more about 'War in the Blood' documentary and research behind it.
Interview with Mellie, Graham's wife, about their story and being part of the 'War in the Blood' documentary published in the Telegraph on 7 July 2019
Scott's story about taking part of a CAR T-cell trial at University College London Hospital (UCLH) published in The Daily Mail on 1 July 2019
- Tanya's story about being the third pateint receiving CAR T-cell therapy to fight leukemia published in The Daily Mail on 29 October 2018
Breakthrough cell therapies treating blood cancers
Professor Karl Peggs
Early results from the COBALT trial and other studies show that aggressive cancers can be tamed with CAR-T therapies which re-engineer the body’s immune system to seek out and neutralise abnormal and malignant cells.
“Our early process was very labour intensive with lots of people gowned up and working one step at a time, which meant we could not make many products and that it was costly,” says Professor Karl Peggs, project leader and scientific director of the National Institute for Health Research Blood and Transplant Research Unit in Stem Cells and Immunotherapies.
“We realised that we needed to create an automated process that could be performed in closed systems without manufacturing in such a high-dependency and high-cost manufacturing environment. Our work has enabled us to reduce cost and complexity significantly, with multiple machines in a single room each capable of manufacturing a dose of cells. Our early trials taught us an awful lot and established important infrastructure. With that knowledge and processes in place, we can look at fresh ideas and new patient groups that might benefit.
“Thanks to our funders, we are now in a very good position to take other academic programmes forward, while industry partners are much keener to work with us to run big international trials and this means we get more access to new therapies for UK patients through commercial studies.The knock-on effect of our research is that manufacturing is cheaper and more efficient with far lower failure rates. Rather than treating one patient per month, we can now make multiple products and treat a lot more patients. The ability to be able to offer therapies patients cannot get elsewhere is hugely important.
University College London Hospitals recently announced a partnership with the Exilarch’s Foundation to develop Europe’s first unit dedicated to delivering these therapies, the Sir Naim Dangoor Centre for Cellular Therapy.
Improving cancer treatment is “major priority” for public

Image credit: Roswell Park Comprehensive Cancer Center
Enhancing cancer treatment is a “major priority” for the UK public, which also thinks that the NHS needs more resources to provide “excellent cancer care”, finds a new national survey led by UCL.
The study, British Public Attitudes towards Cancer Research and Treatment in 2019, found that half (49%) the population believe cancer is the disease group for which they most want better treatments for themselves and their families. In addition, 59% believe that stopping the suffering caused by cancer is one of the most important things society could achieve by 2050. Read on
 Close
Close

