Insights on including Patient and Public Involvement (PPI) in Advanced Therapies
6 May 2021
The Cell & Gene Therapy and Regenerative Medicine TINs presented an online event to highlight the importance of Patient and Public Involvement (PPI) in translational research.
In a recent Therapeutic Innovation Networks (TINs) seminar jointly hosted by the Cell & Gene Therapy and Regenerative Medicine TIN, insights were provided on how Patient and Public Involvement (PPI) improves the quality, strength and relevance of such projects, as well as how to get involved.
With a particular focus on advanced therapies, the seminar welcomed the varied perspectives of leading researchers, clinicians and patients in PPI, outlining the importance to research and highlighting the real-world impacts.
Bringing researchers, patients and public together for mutual learning to support patient-centric research
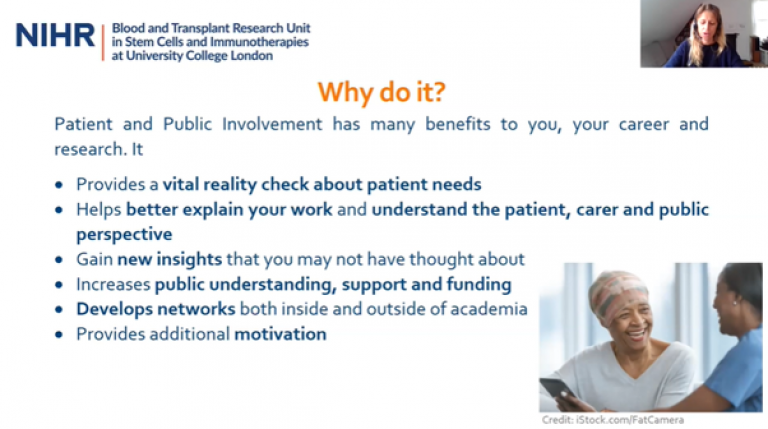
The first speaker, Linda Von Neree (PPI Lead at NIHR Blood and Transplant Research Unit (BTRU) in Stem Cells and Immunotherapies at UCL) gave an overview of PPI and the benefits, as well as how to approach the PPI section commonly found in translational funding applications. Linda mentions that a common misconception of PPI is simply participation, when rather, PPI is much more than that, and should involve a two-way conversation and a mutually beneficial relationship.
A key message throughout the talks is the cruciality of including PPI early on in translational research to maximise research. This is first mentioned by Linda when discussing PPI in funding applications. Including patient and public involvement as early as possible not only demonstrates to funders that you have awareness of needs for a patient-centric strategy and the costs involved, but also allows you to build a relationship with patients to meet these needs by incorporating them into your novel therapeutics to increase chances of clinical uptake.
For more information about including PPI in your advanced therapies research, please contact Linda Von Neree, Translational Research Office (TRO).
Are patients willing to have gene therapy?
Professor Matthew Walker (Consultant Neurologist at the National Hospital for Neurology and Neurosurgery) spoke as the first panellist representing an academic researcher perspective, highlighting his involvement of patients in his own gene therapy research on epilepsy. Professor Walker describes how PPI has been important throughout his studies – from initially, determining if patients were willing to have gene therapy as a treatment option for epilepsy, through to providing clarity and reassurance to the public about the new therapies developed. This is especially relevant for cell and gene therapy where viral vectors are injected into the body, which can cause some concern for patients. Therefore, another key area for involving patients, is in drawing up the patient information literature to provide an accurate representation of the therapy in lay language, is an incredibly important factor for successful clinical trial recruitment.
Professor Walker also highlights the type of characteristics to look out for when determining “who” should get involved. His talk runs between 17:34 and 29:02 in the recording link below:
Watch the PPI event webinar recording
Additionally, if you would like to learn more specifically about Professor Matthew Walker’s work and the portfolio of supporting gene therapy projects that it is a part of, please take a look at our recent TRO 10-year review, which highlights this key work supported by the TRO as a case study on page 21: https://bit.ly/2TRO10
Gene therapy trials – the patient perspective
As the event agenda turned to the patient perspective, Luke Pembroke showed an impactful video to describe his personal experience as a Haemophilia B gene therapy patient:
Watch the PPI event webinar recording
Involving PPI in Pre-Clinical Work
Final speaker, Dr Nick Hamilton (NIHR Clinical Lecturer, UCL), brought us back round again to the importance of including PPI early in research, even in pre-clinical stage work.
As an ENT surgeon, Dr Hamilton’s work involves problems within the throat and looking at the delivery of mesenchymal stem cells to help overcome these. The cells used are taken from the discarded umbilical cord following birth and are grown in the lab before being delivered to the patient. Something that he thought about when starting this project, was “how will people feel about having these cells taken from that source?”. Dr Hamilton set out to get that early opinion with the guidance of the UCL Translational Research Office. Running a focus group provided the opportunity to adapt and change his therapies before getting locked into a way of doing things that perhaps wasn’t suitable for patients.
I’m a big believer that we should start to think about PPI early in the translational process, and not wait until it’s too late to engage”.
The presentations were followed by a poll of the audience and an insightful panel discussion with Q&A. To view the full event recording, please complete the form via the link below and join the Cell & Gene Therapy and Regenerative Medicine TINs if you would like to attend future events.
- View the recording of “C&G/RegMed TIN: Patient and Public Involvement (PPI) in Advanced Therapies”
- Join a Therapeutic Innovation Network (TIN)
If you would like to get in touch with any of the speakers and/or explore possible collaborations with regard to the topics discussed, please contact TIN Coordinator Dr Asha Recino (a.recino@ucl.ac.uk).
Further resources for Patient and Public Involvement (PPI) in research
- UCL Hospitals Biomedical Research Centre (UCLH BRC) PPI training, https://www.uclhospitals.brc.nihr.ac.uk/investigators/ppi/at-a-glance
- NIHR INVOLVE online training and other PPIE resources, https://www.invo.org.uk/resource-centre/learning-and-development/public-reviewing-with-the-national-institute-for-health-research-nihr/#top
- UCLH BRC: ‘A practical guide to patient and public involvement in lab-based research’, https://sites.google.com/parkinsons.org.uk/ppi-in-lab-based-research/home
- PPI in CAR-T study ‘Partnering with patients to get better outcomes with chimeric antigen receptor T-cell therapy: towards engagement of patients in early phase trials’, https://researchinvolvement.biomedcentral.com/articles/10.1186/s40900-020-00230-5
- ACCELERATE Expertise resources on involving patients and the public in research
UCL(H) PPI Leads
- UCL Blood and Transplant Research Unit, l.vonneree@ucl.ac.uk
- UCL Great Ormond Street Institute of Child Health, research.ppi@gosh.nhs.uk
- UCLH BRC, ppihelpdesk@ucl.ac.uk
- Moorfields BRC, h.baker@ucl.ac.uk
 Close
Close

