Insight into immune cell activation could help identify Covid-19 patients most at risk of pneumonia
12 October 2020
Researchers have identified an immune response detectable in the blood of patients with Covid-19 that could be used to determine whether a patient with the virus will develop severe lung complications.
The study, published in the International Journal of Infectious Diseases (IJID), found that by examining levels of a protein molecule known as Complement Receptor 3 (CR3) in immune cells, they could distinguish Covid-19 patients with pneumonia from those with mild symptoms. The study also offers insight into how Covid-19 related lung damage might be treated.
Covid-19 – the disease caused by the SARS-CoV-2 virus - affects the body in different ways. Most infected people will experience mild to moderate disease, while others will progress to severe or critical disease, including pneumonia and acute respiratory failure. It is thought that the body’s initial immune response to the virus plays a large part in how severe the disease becomes i.e. people with an overly reactive immune response are more likely to become seriously ill with Covid-19.
To understand more about the reasons why some patients with Covid-19 develop pneumonia and others do not, Dr Rajeev Gupta and research colleagues from UCL and UCLH profiled circulating monocytes (a type of white blood cell of the immune system) from a cohort of adult patients with Covid-19 and specifically compared those with mild symptoms with those who had developed pneumonia.
The team found that levels of the CR3 protein were higher in the monocytes of Covid-19 patients who had developed pneumonia compared with those who did not. CR3 is central to immune activation and helps coordinate the body’s response against infection and triggers inflammation. It is also an active component of blood clotting within the body.
“We saw striking and unexpected differences in the cells of the innate immune system. Levels of CR3 were increased in monocytes from Covid-19 patients experiencing respiratory failure, but not in those with Covid-19 who remained well, or those without Covid-19 but ventilated for other reasons. We also saw that Natural Killer (NK) cell numbers were two-fold higher than normal in Covid-19 patients who remained well,” explains Dr Rajeev Gupta, Clinical Associate Professor (UCL), Consultant Haematologist (UCLH) and lead author of the study.
“Our findings suggest tracking of CR3 expression and NK cells in individual patients with COVID-19 as potential biomarkers for disease severity. By identifying which infected individuals are at risk of severe illness at an early stage we could plan treatment accordingly. Our study also suggests that targeting of CR3 with drugs such as Colchicine or Simvastatin could be an effective way to prevent or treat COVID-19 pneumonia. And in the absence of an effective vaccine, preventing lung failure in Covid-19 patients would be an ideal intervention.”
This study was funded by UCL Biomedical Research Centre’s emergency COVID-19 funds and Blood Cancer UK. Supported by philanthropic donations from Sir Peter Wood and Cure Cancer @ UCL.
Further information
- Research paper: Increased Complement Receptor-3 levels in monocytes and granulocytes distinguish COVID-19 patients with pneumonia from those with mild symptoms, International Journal of Infectious Diseases.
- Dr Rajeev Gupta academic profile
- UCL Stem Cell Lab - Prof Tariq Enver
- UCL news: Real-time pneumonia test for Covid-19 patients aiding faster therapy
- UCL news: Scientists aim to unravel immune system’s response to COVID-19
- UCL Media Team contact: Henry Killworth h.killworth@ucl.ac.uk
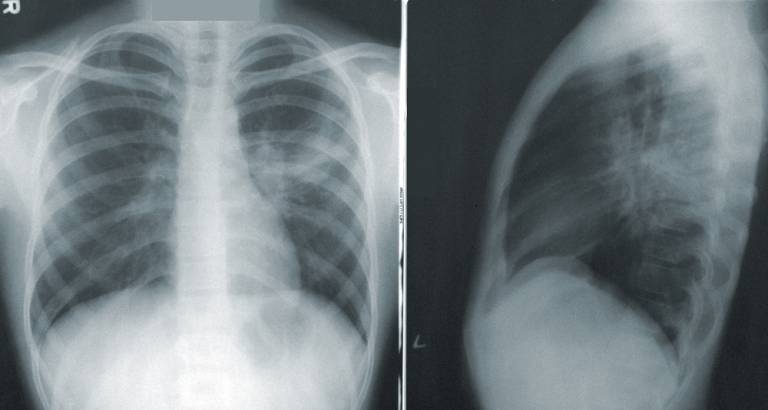
- Main image: X-ray showing Pneumonia. Photo by CDC on unsplash
 Close
Close

