Timeline of the PETAL Programme
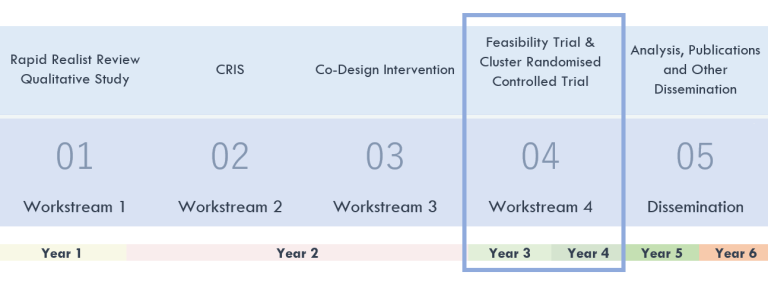
See below for more information on each study phase
- Workstream 1: Rapid Realist Review and Qualitative study
Workstream 1a: Rapid Realist Review
We looked at previous research to see what works in therapy programmes for aggressive challenging behaviour, for whom and in what circumstances. We looked at information from 59 research studies, including people with conditions such as learning disability, autism spectrum disorder and dementia, in the community and inpatient settings. This work helped us develop theories explaining how therapies may work in these populations and settings.
Emerging theories include:
- emotion regulation and skill development, sensory stimulation and meaningful activities for people with learning disabilities
- enhancing family and paid carer skills and efficacy
- understanding and listening to those receiving therapy, personalising session delivery
- mentoring and supporting therapists
- improving communication with paid and family carers
The rapid realist review has been published in the journal PLOS One (see dissemination page for access to the paper). An accessible summary of the paper has also been published as an NIHR alert. Click here to read.
Workstream 1b: Qualitative interviews
We explored barriers and facilitators that influence responses to psychological therapy in adults with learning disabilities who display aggressive challenging behaviour.
We completed 42 interviews with adults with mild/moderate learning disabilities, family and paid carers, and other social care professionals from 7 sites across England, Scotland, and Northern Ireland. We asked about their experiences with therapies and why they thought their outcomes were good or less favourable.
Key themes relating to positive therapy outcomes were the following:
- therapeutic alliance such as staff consistency, developing rapport and relationships, involvement of adults with learning disabilities and carers in care planning
- streamlining and collaboration of support between staff
- person-centred support and environment
- engagement in meaningful activities and relationships
The main barriers to positive outcomes were structural and organisational issues such as inadequate support, lack of resources and organisational culture and attitudes.
This work has been published in NIHR Open Research (see dissemination page for access to the paper).
- Workstream 2: CRIS (Clinical Record Interactive Search)
This work aimed to identify whether some people are more likely to come to contact with crisis services due to display of aggressive challenging behaviour and to explore what happens as they move through the services.
We analysed routinely collected NHS data through a mental health database called CRIS (Clinical Record Interactive Search). The results showed that people who present aggressive challenging behaviour were more likely to contact such services if they:
- had a diagnosis of a personality disorder or common mental health disorder (e.g., anxiety, depression), if they experienced episodes of agitation and
- were having more contact with professionals in mental health services. People with neurodevelopmental conditions (e.g., autism spectrum disorders, developmental language disorder, learning disability, motor disorders), however, were less likely in need of crisis support.
This work has been published in the journal European Psychiatry (see dissemination page for access to the paper).
- Workstream 3: Development of the PETAL therapy
The PETAL personalised therapy was developed with the active involvement of our advisory groups of adults with a learning disability, family and paid carers. Seven co-production meetings were held between July 2021 and April 2022 to design the PETAL therapy. The PETAL therapy was also informed by the findings of Workstreams 1 and 2.
We have developed the PETAL therapy manual for therapists, workbooks for adults with learning disabilities and carers, and a training programme for PETAL therapists. The PETAL therapy will be delivered flexibly over 14 weeks. It includes modules on understanding behaviour, improving communication, emotional regulation, calming/relaxation activities, carer well-being and healthy habits.
- Workstream 4: Feasibility study
We are now reaching the end of the feasibility phase. So far, it has helped us understand whether the PETAL therapy is acceptable, whether it could be delivered as planned and whether there are any barriers or facilitators to the therapy within the NHS services. This allowed us to generate the best version of the PETAL therapy so we can test in the full-scale trial.
The feasibility phase started in February 2023. Six NHS trusts from England finished participation in the feasibility trial and one from Scotland is still currently running. These trusts are:
- Camden and Islington NHS Foundation Trust
- East London NHS Foundation Trust
- Livewell Southwest
- Nottinghamshire Healthcare Trust
- Barnet, Enfield and Haringey Mental Health Trust
- Cheshire and Wirral Partnership NHS Foundation Trust
- Greater Glasgow and Clyde NHS Trust
15 therapists joined two therapist training days which were held in January and March 2023.
10 people with a learning disability and their (family or paid) carers have taken part in the feasibility trial.
As part of the feasibility assessment, we have completed interviews with carers, people with learning disability, therapists, supervsiors, and service managers.
We are continuing to collect these interviews to see how the therapy went and if there is anything we could to the PETAL therapy to improve it for the full trial.
- Workstream 4: The PETAL trial
The PETAL trial will examine if PETAL therapy reduces aggressive challenging behaviour in adults with learning disabilities. We will also test if the PETAL therapy is value for money compared to what is currently available for adults with learning disabilities and their carers in the NHS.
We have invited 41 NHS teams from England, Scotland and Northern Ireland. 11 NHS teams have already agreed to take part. Overall, we aim to recruit 410 adults with learning disabilities and their carers. Each service will be randomly assigned (i.e., by chance) to either receive 1) the PETAL therapy along with usual care or 2) usual care alone. Comparing the outcomes between services that received or did not receive the therapy will help us understand whether PETAL therapy is clinically and cost-effective. If indeed it is found effective, PETAL therapy can help change our current practices to better support adults with learning disabilities who display aggressive challenging behaviour and improve their quality of life.
The full-scale trial started in January 2024. We currently have 6 sites which are open to recruitement. More sites will be opening soon. Some sites have already recruited participants.
To take part in the study, participants and services will have to meet the following inclusion and exclusion criteria:
Inclusion Criteria Exclusion Criteria Participants - Aged 18+ years old or over
- Living in the community (e.g., residential care home, supported living, family home)
- Registered with and/or eligible to receive support from community learning disability services. It is likely that people will have several additional comorbid behaviours such as verbal aggression, mental health problems, self-injury, stereotypies etc.
- Incidents of physically aggressive behaviour (e.g., to people or property) for at least 3 months
- Capacity to consent or assent from family/nominated consultees for those lacking capacity
Family carer/other members able to understand English
- Primary substance misuse
- Current enrolment in another clinical trial
- Being an inpatient
Services - Community Intellectual Disability Service(s) able to complete capacity and capability assessment
- Staff available and willing to train in and deliver the intervention
- Community Intellectual Disability Service(s) unable to complete capacity and capability assessment
- No staff available to train in and deliver the intervention
 Close
Close


