Clinical trial co-led by UCL leads to new bowel cancer drug approval
14 May 2021
Cancer researchers at UCL, involved in an international trial which found that pembrolizumab more than doubled the ‘progression free survival’ of patients with a subtype of bowel cancer, when compared with chemotherapy, are delighted it has now been approved by the UK regulator.
Today (Friday May 14) the National Institute for Health and Care Excellence (NICE) published draft guidance recommending pembrolizumab, a form of immunotherapy, as a first-line treatment option for adults with previously untreated metastatic colorectal cancers with high levels of microsatellite instability (MSI-H) or DNA mismatch repair deficiency (dMMR).
This announcement follows the ‘KEYNOTE-177’ Phase III clinical trial, which found patients who were treated with pembrolizumab (also known as Keytruda) had ‘progression-free survival’ of 16.5 months (on average), compared with 8.2 months for those who were treated with chemotherapy.
‘Progression free survival’ is the length of time during and after the treatment of a disease, such as cancer, that a patient lives with the disease but it does not get worse. In a clinical trial, measuring the progression-free survival is one way to see how well a new treatment works
In addition, 11% of patients who were treated with pembrolizumab were also found to have a ‘complete response’ where their disease had disappeared from scans. Furthermore, in almost half the patients who had pembrolizumab (48.3%), their disease had not progressed after two years versus only a fifth of patients who had had chemotherapy (18.6%), which means the beneficial effects are also durable.
The trial’s UK Chief Investigator, Dr Kai-Keen Shiu, Honorary Associate Professor in Oncology at UCL Cancer Institute and Consultant Medical Oncologist at UCLH, said:
“It is great news for patients that NICE have approved pembrolizumab as first line treatment for metastatic MSI-H/dMMR bowel cancer based on the results of this international trial.
“I am glad that we can now offer eligible patients a therapy which has been shown in the KEYNOTE-177 trial not only to be more effective in stopping tumours from growing versus chemotherapy, but is also shown to have more manageable side-effects. For some patients, access to this treatment could be truly life changing.
“This treatment represents a new standard of care as well as a benchmark for ongoing and future MSI-H/dMMR metastatic colorectal cancer trials.”
The ‘KEYNOTE-177’ Phase III clinical trial, published in the New England Journal of Medicine and funded by Merck & Co (known as MSD in the UK), recruited 307 patients with metastatic bowel cancer, who had specific DNA mutations known as microsatellite instability high (MSI-H) or mismatch repair deficiency (dMMR).
These genetic alterations result in cells being unable to repair themselves correctly if damaged, and when this happens, errors in the DNA accumulate which may cause cancer. MSI-H/dMMR can be hereditary (also known as Lynch Syndrome) or sporadic, and affected patients usually have a poor prognosis when the disease has spread to other organs.
The randomised controlled trial recruited patients from 23 countries who were put into two equally sized groups. One group (or arm) of patients received pembrolizumab every three weeks for up to 35 cycles of treatment (up to approximately two years), while the other group received standard chemotherapy combinations with cancer targeting drugs bevacizumab or cetuximab (the chemotherapy arm) every two weeks.
University College London Hospitals NHS Foundation Trust (UCLH) was one of the largest recruiters of patients for the trial with 18 participants from across England and 10 patients received pembrolizumab as first-line treatment.
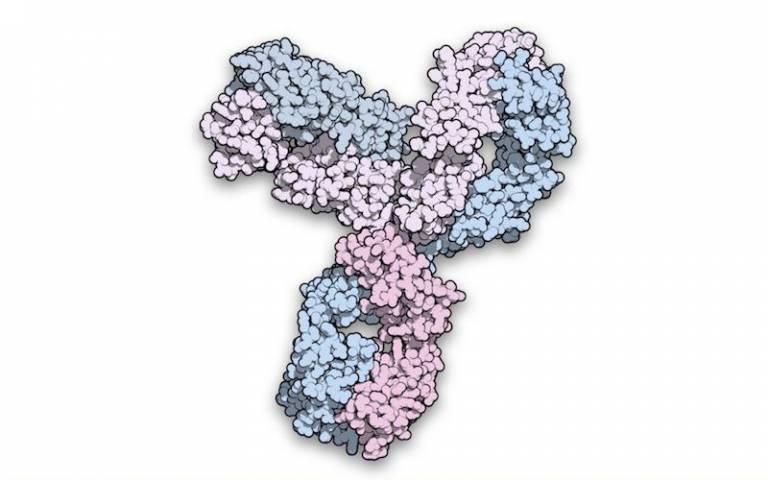
Pembrolizumab is a type of immunotherapy known as a check-point inhibitor and helps make cancer cells more vulnerable to attack by your body’s own immune system. It does this by blocking the activity of a molecule called PD-1, thereby allowing T cells (white blood cells that help your body fight disease) attack and kill tumours as they should.
NICE are expected to publish the final guidance on pembrolizumab in June 2021.
Links
- NICE guidleines on pembrolizumab
- KEYNOTE-177 trial results published in the NJEM
- Dr Kai-Keen Shiu’s academic profile
- UCL Cancer Institute
- UCLH
- MSD
Image
- 'Space-filling model of pembrolizumab', on wikimedia commons. CC BY 2.0
Media Contact
Henry Kllworth
Tel: +44 (0) 7881 833274
 Close
Close

