Analysis: Covid-19 - How to triage effectively in a pandemic
9 March 2020
Triage in a pandemic is even thornier than you might think, write Professor Christina Pagel (UCL Mathematics) and colleagues for the BMJ.

The UK is likely on the brink of a major covid-19 outbreak. [1,2] About 6%-10% of infected people are likely to be critically ill, most of whom will require ventilation support in an intensive care environment. [3,4] Italy is already experiencing extreme stress on its intensive care system and in a matter of weeks the UK too may be facing a situation where demand for intensive care exceeds capacity (for instance there are around 4100 beds in England [5]). The NHS urgently needs to address the question of how access to intensive care is determined when there are not sufficient resources to treat everyone.
The default when demand for services outstrip supply is first-come first-served, where resources are locally allocated on the principle of “next in line” and no one is excluded a priori. Triage protocols are designed to promote a more rule-based system for allocating scarce resources fairly and transparently, where, by definition, some groups of people are excluded from access to care. Various protocols for triage to intensive care have been suggested for use in a pandemic. [4,6,7]
Prior to and during the 2009 H1N1 flu pandemic, we undertook mathematical modelling to understand the circumstances under which triage led to higher population survival. [8] Some of the things we learned are highly relevant for the current situation, so below we offer key considerations for the NHS before implementing any triage protocol.
Why triage? What are you trying to achieve?
Although some triage protocols focus on excluding some patients to increase availability of intensive care beds, bed availability is not an end in itself. [6] The implicit (and sometimes explicit) intent of triage protocols tends to be the “public good” of maximising population survival. Ideally, there would be society-wide conversation about whether this should be the goal of triage in a pandemic, but for covid-19, it is too late. However, if the NHS does decide to implement triage to intensive care, the “public good” purpose needs to be made explicit and transparent.
What is the scarce resource you are trying to maximise?
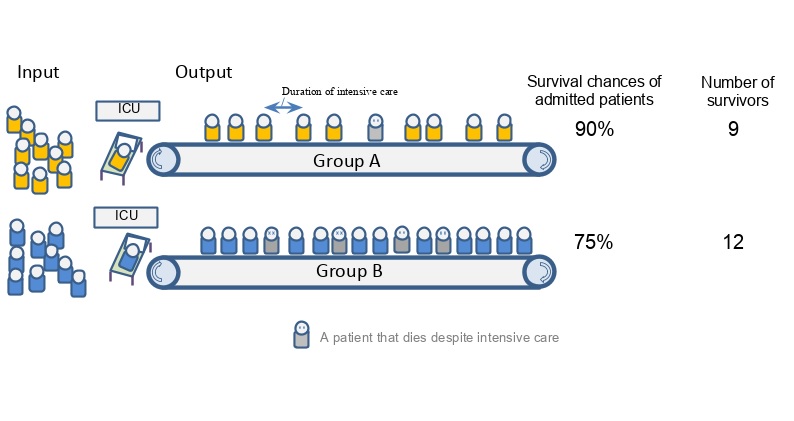
A key insight from our work is that it is wrong to assume that this public good is achieved by maximising survival among those that are granted intensive care. While many triage protocols acknowledge this by aiming to exclude patients who don’t absolutely need it (the “too well”) as well as those least likely to benefit (the “too sick”), they don’t pay enough attention to differences between groups in terms of the duration of intensive care required to achieve outcomes. The figure below illustrates this point.
Many triage protocols would favour admission of group A over group B because patients in group A have a higher chance of survival if given intensive care. However, in this example, patients in group B require shorter length of stay on ICU than patients in group A and so allocating intensive care resource to group B actually leads to a higher absolute number of survivors, because more people get access to life saving care. If the aim of triage is to best enhance population survival with a scarce resource, then the scarce resource is not beds, but bed-days; it is not ventilators, but ventilator-time.
Is effective triage even possible?
Any triage protocol depends on excluding some patients from intensive care. It follows that triage will not be effective if the vast majority of people requiring intensive care have a similar chance of survival and a similar anticipated length of stay. While the typical UK ICU population is very heterogeneous, during a pandemic caseload will be dominated by covid-19 cases, and it is possible that little meaningful differentiation will be possible.
Even if there is a subgroup of patients whose exclusion would lead to higher population survival, can you reliably tell them apart in advance? If not, then triage will again be ineffective. Even if you could meaningfully distinguish groups of patients at a population level, if the spreads of survival probability and/or lengths of stay overlap a lot between the groups, then any given individual from the group to be excluded might in fact have higher chances of survival or a shorter stay than any given one from the included group—how comfortable would clinicians feel in denying care to the patient identified for exclusion? How accepting would the public be of such decisions, particularly when it affects them or their loved ones? How big does the population level survival benefit have to be to balance the potential societal costs associated with a loss of trust in the NHS?
Summary
Pragmatically, a first-come first-served approach to access will be hard to escape. This approach may be the fairest way to allocate care at a population level—every citizen has a roughly equal chance of accessing care when they need it although in practice it might well disadvantage the more vulnerable in society with the worst access to healthcare. While triage may be an effective way to increase population survival, this is not guaranteed and any protocol should be carefully thought through.
Politicians and clinical leaders will stress that decisions on triage protocols are tough decisions to make, and they are right. But they are tougher decisions to implement and tougher still to be on the receiving end of. Any triage protocol will lead to tragic choices for some. This should not be left as the responsibility of individual clinicians without guidance from the NHS, the Royal Colleges, and Professional Societies to ensure consistency, equity and transparency. We’ve arguably missed the opportunity to properly engage the public in decisions on how we use their scarce resources to their benefit, but efforts must be made to ensure that the public understand the purpose of any triage protocol and how it will be applied, and are able to trust that it will be consistently applied.
There is no single right answer, but if containment and delay measures fail then the NHS needs to find an answer and soon. [3] And when covid-19 is over, we need to start the conversations with the public for next time.
Links
- Article in BMJ Blogs
- Professor Christina Pagel's academic profile
- UCL Mathematics
- UCL Mathematical & Physical Sciences
Image
- Professor Christina Pagel
 Close
Close