Poorest countries facing ‘double burden’ of obesity and malnutrition
16 December 2019
More than one in three low- and middle-income countries are facing high levels of obesity and under-nourishment, according to a report involving UCL researchers.
The report, published today in The Lancet, says a new approach is needed to help reduce the ‘double burden’ of undernutrition and obesity at the same time, as the issues become increasingly connected due to rapid changes in countries’ food systems.
This is especially important in low- and middle-income countries, according to the new four-paper report. More than a third of such countries had overlapping forms of malnutrition (45 of 123 countries in the 1990s, and 48 of 126 countries in the 2010s), particularly in sub-Saharan Africa, south Asia, and east Asia and the Pacific.
Co-author, Professor Jonathan Wells (UCL Great Ormond Street Institute of Child Health) said, “Until recently, the double burden of malnutrition was something that was considered to affect populations, or perhaps households, for example, where an overweight mother has a child who experiences a slower rate of growth.
“But the speed with which our food environments are changing means that an increasing number of people are exposed to different forms of malnutrition at different stages of life. A growing number of those who develop obesity, from childhood onwards, also experienced under-nutrition early in life. That’s a double burden for the individual, and it increases the health costs of obesity, making people more vulnerable to diabetes, heart disease and stroke.
“We can no longer make a simple separation between under-nutrition and being overweight, the two forms of malnutrition both contribute to poor health, and we need to fundamentally improve our food systems and diets in order to counter this.”
Globally, estimates suggest that almost 2.3 billion children and adults are overweight, and more than 150 million children are stunted. However, in low- and middle-income countries these emerging issues overlap in individuals, families, communities and countries. The new report explores the trends behind this intersection – known as the double burden of malnutrition – as well as the societal and food system changes that may be causing it, its biological explanation and effects, and policy measures that may help address malnutrition in all its forms.
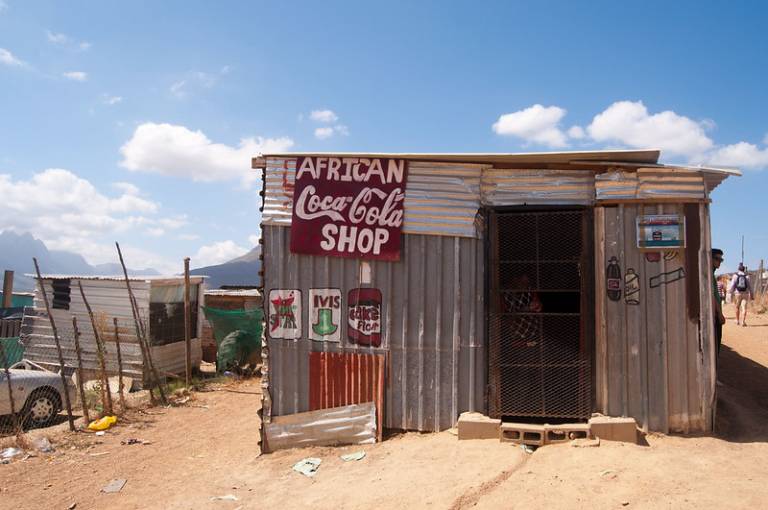
“We are facing a new nutrition reality,” said lead author of the report Dr Francesco Branca, Director of the Department of Nutrition for Health and Development, World Health Organization. “We can no longer characterize countries as low-income and undernourished, or high-income and only concerned with obesity. All forms of malnutrition have a common denominator – food systems that fail to provide all people with healthy, safe, affordable, and sustainable diets. Changing this will require action across food systems – from production and processing, through trade and distribution, pricing, marketing, and labelling, to consumption and waste. All relevant policies and investments must be radically re-examined.”
The authors used survey data from low- and middle-income countries in the 1990s and 2010s to estimate which countries faced a double burden of malnutrition (ie, in the population, more than 15% of people had wasting, more than 30% were stunted, more than 20% of women had thinness, and more than 20% of people were overweight).
In the 2010s, 14 countries with some of the lowest incomes in the world had newly developed a double burden of malnutrition, compared with the 1990s. However, fewer low- and middle-income countries with the highest incomes were affected than in the 1990s. The authors say that this reflects the increasing prevalence of being overweight in the poorest countries, where populations still face stunting, wasting and thinness.
Professor Wells added: "It’s easy to assume that the risk factors for under-nutrition and overweight are very different, but we are starting to realise that actually, they are often the same factors. For example, highly processed foods are often very energy-dense but don’t satisfy hunger very well, and so they contribute to excess weight gain. But the same foods are also often low in micronutrients, and so they can contribute to micronutrient deficiencies, and to poor growth in young children.
“Also, how we eat is subject to many unhealthy commercial interests. People who are less well-off are pushed towards buying these cheap processed foods and drinks, and these products are obviously designed with a view to maximising sales, not health. If we want to improve health, we need to radically improve access to healthy foods.”
Exposure to undernutrition early in life followed by becoming overweight from childhood onwards increases the risk of a range of non-communicable diseases – making the double burden of malnutrition a key factor driving the emerging global epidemics of type 2 diabetes, high blood pressure, stroke, and cardiovascular disease. Negative effects can also pass across generations – for example, the effect of maternal obesity on the likelihood of the child having obesity may be exacerbated if the mother was undernourished in early life.
The report identifies a set of ‘double-duty actions’ that simultaneously prevent or reduce the risk of nutritional deficiencies leading to underweight, wasting, stunting or micronutrient deficiencies, and obesity or NCDs, with the same intervention, programme, or policy. These range from improved antenatal care and breastfeeding practices, to social welfare, and to new agricultural and food system policies with healthy diets as their primary goal.
Source
Links
- UCL Great Ormond Street Institute of Child Health
- Professor Jonathan Wells' academic profile
- The Lancet papers
Image
Media contact
Rowan Walker
Tel: +44 (0)20 3108 8515
Email: rowan.walker [at] ucl.ac.uk
 Close
Close

