Novel brain imaging methods improve neurosurgical treatment for epilepsy
12 December 2014
Advances in brain scanning at the UCL Institute of Neurology underpinned major improvements in the surgical treatment of epilepsy, reducing the risk of loss of sight, language or control of limbs. This is now used in epilepsy surgery at the National Hospital for Neurology and Neurosurgery and is being rolled out elsewhere.
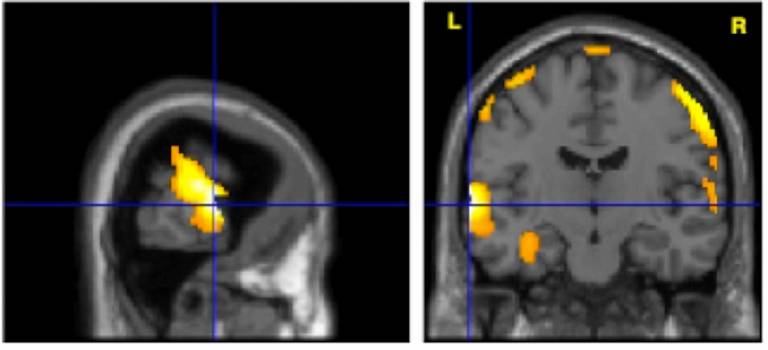
Epilepsy is one of the most common serious brain disorders, affecting over 450,000 people in the UK. One third of these individuals continue to have seizures despite anti-epileptic drug treatment. For those in whom the source of epilepsy can be pinpointed in the brain, neurosurgical treatment can be curative. Over the last 20 years, research led by Professor John Duncan (UCL Institute of Neurology) has optimised brain imaging applied to epilepsy surgery and the clinical utilisation of functional magnetic resonance imaging (fMRI) and tractography to visualise brain activations related to language, motor and sensory functions and memory, and critical nerve pathways in the brain.
The fMRI and tractography approaches pioneered at UCL are now used by neurosurgeons throughout Europe to identify the risks of surgery in individuals, and to plan the surgery so that risks may be reduced. Surgeons use tractography to visualise pathways of white matter fibres in the brain in the pre-operative MRI scans, helping them to avoid damaging nerve fibre pathways, which can otherwise lead to visual impairments that would, for example, prevent driving. The system is used on roughly one patient a week and it has been fully operational since 2012.
As well as informing decisions about whether to undertake surgery or not, scans are also used in the interventional MRI operating theatre during surgery. A three-dimensional map of critical brain areas can now be visualised and presented to the surgeon as the operation proceeds, to enable the guiding of the surgery away from critical areas that must be avoided. This enhancement is already used in clinical practice at the National Hospital for Neurology and Neurosurgery, resulting in safer surgery with reduced risk of causing new visual impairments.
An early evaluation of the system demonstrated its impact in 21 patients undergoing anterior temporal lobe resection compared to a control group who underwent the same surgery without the system. None of those who had their visual pathway displayed to the surgeon via the tractography system were left with a visual impairment that would prevent driving, compared to 13% in the control group.
The use of fMRI to identify the side of the brain responsible for this function has entirely replaced the carotid amytal test at the National Hospital for Neurology and Neurosurgery, with benefits to patients and health providers. The old, more expensive test could be dangerous, involved radiation and required a two-day hospital stay. The hospital used to carry out around four such procedures per month, but have done none since 2004. The fMRI method has been widely adopted in epilepsy surgery centres around the world.
A specific example of the dramatic impact of imaging technology was of a 28-year-old man with severe epilepsy that was not controlled by medications. While standard MRI scan showed nothing, computerised analysis identified an abnormal area. Functional MRI scans further showed this was near areas involved in language and abutting parts controlling the right arm. Tractography showed that the corticospinal tract, which carries command and control information to the limbs, ran within a few millimetres of the abnormal area. These data allowed the precise positioning of recording electrodes in and around the abnormal area and led to precise surgical removal of the part of the brain that was giving rise to the seizures. As a result, no further seizures have occurred, medication has been withdrawn, and the patient is going to college and learning to drive. For many such individuals, the impact of this research was immediate and life changing.
The UCL Institute of Neurology's focus on MRI applied to epilepsy contributed to the development of epilepsy imaging protocol guidelines by the International League against Epilepsy, between 1998 and 2011. These underpinned the imaging guidelines for epilepsy that were used in the National Institute for Health and Clinical Excellence (NICE) epilepsy guidelines of 2004 and 2012.
Related links
- Winston GP, Daga P, White MJ, Micallef C, Miserocchi A, Mancini L, Modat M, Stretton J, Sidhu MK, Symms MR, Lythgoe DJ, Thornton J, Yousry TA, Ourselin S, Duncan JS, McEvoy AW. Preventing visual field deficits from neurosurgery. Neurology. 2014 Aug 12;83(7):604-11. pii: 10.1212/WNL.0000000000000685. [Epub ahead of print] PubMed PMID: 25015363. UCL Discovery.
Image
- Auditory naming activation
 Close
Close

