Find out about the Dr Alex Shortt's research on bioengineered stem cell transplants.
Corneal stem cells transplants inevitably interact with the recipient patient’s immune system. The aim of this research is to investigate how these two biologically distinct cell types recognise and interact with one another. We hope to find ways of promoting the beneficial interactions and preventing the undesirable ones so that we can treat more patients with severe forms of corneal blindness.
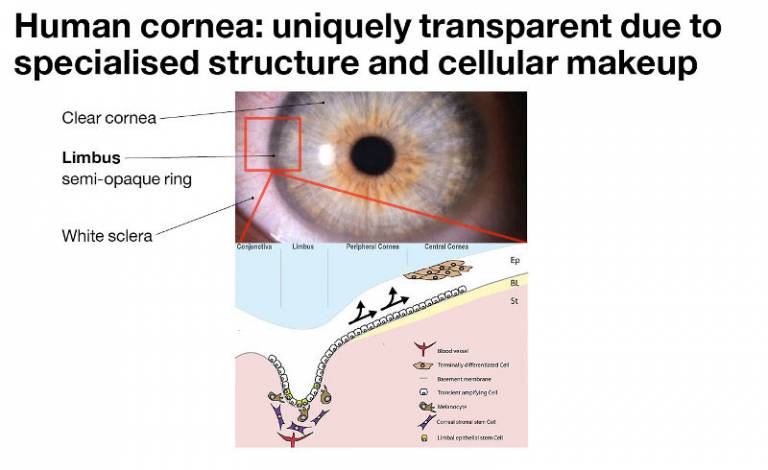
The limbus is the repository of two populations of stem cells that are essential for vision. It contains a host of important structures such as nerves, blood vessels, melanocytes and, most importantly, two kinds of stem cells: Limbal Epithelial Stem Cells and Corneal Stromal Stem Cells. Limbal stem cells are responsible for regenerating the cornea throughout life, be that replacing cells that are lost through day to day wear and tear or by regenerating the cornea following injury.
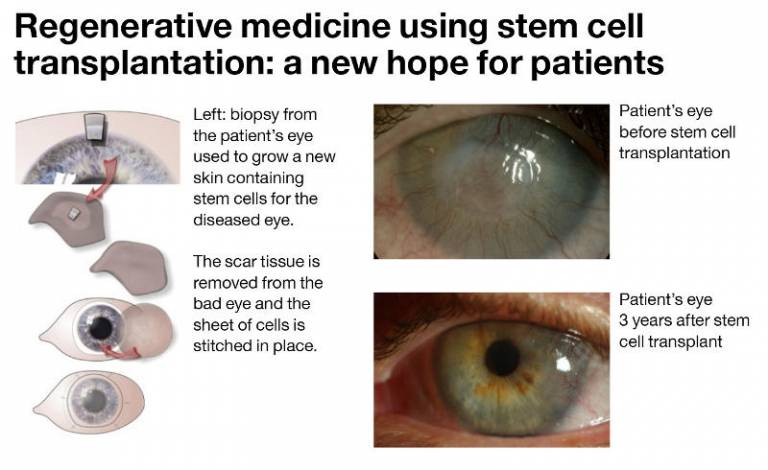
Scientists discovered that the limbus contains stem cells in the 1980s. Since the 1990s surgeons and scientists have been working on treating patients with limbal stem cell damage using stem cell transplants. The photographs here show the successful result of stem cell transplantation treatment in one patient’s eye. The patients own corneal stem cells were used, taken from his healthy eye.
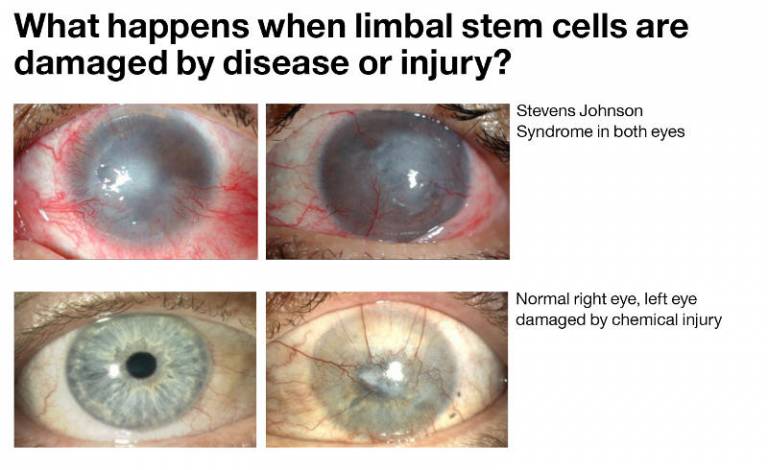
Above: Stevens Johnson Syndrome – the limbal stem cells in both eyes have been destroyed and the patient is blind. Below: Left eye damaged by a chemical injury – cement dust blew into the patient’s eye on a building site resulting in a severe chemical burn to the surface of the eye. The limbal stem cells have been destroyed and the corneal has lost its transparency. The eye is painful and effectively blind.
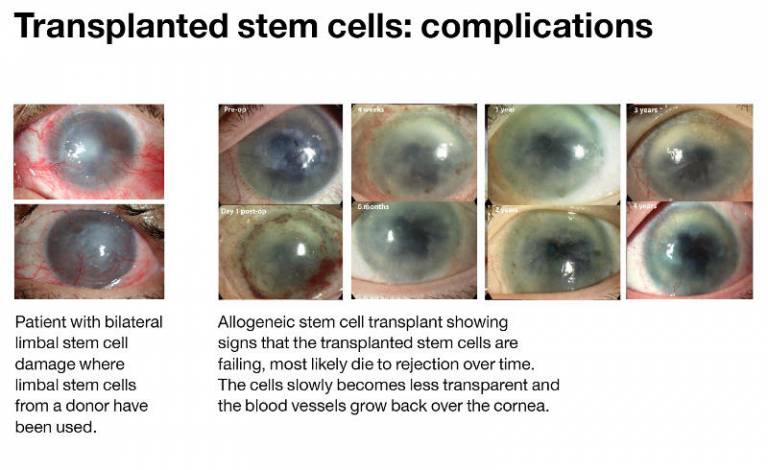
In patients with bilateral limbal stem cell damage it is not possible to use their own cells. Therefore limbal stem cells from a donor, either living or deceased are used. The problem with using donor cells is that the body’s immune system sees these cells as ‘foreign’ and attacks or ‘rejects’ them. This means that the results of limbal stem cell transplants using ‘foreign’ or allogeneic donor cells are not as good as those using the patient’s own cells.
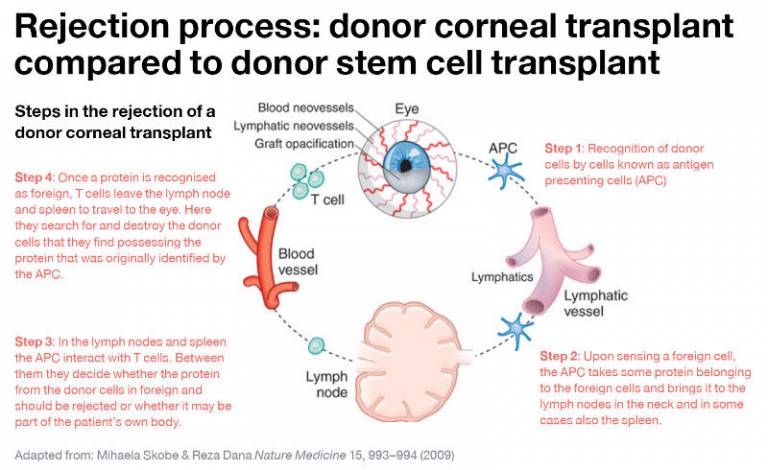
We are investigating whether the same steps operate in the rejection of donor stem cell transplants. Clinically, the rejection of corneal cell or tissue transplants is characterised by the presence of inflammation, the growth of blood and lymphatic vessels into the donor graft and the loss of normalcorneal transparency.
We are investigating whether the same steps operate in the rejection of donor stem cell transplants. Clinically, the rejection of corneal cell or tissue transplants is characterised by the presence of inflammation, the growth of blood and lymphatic vessels into the donor graft and the loss of normalcorneal transparency.
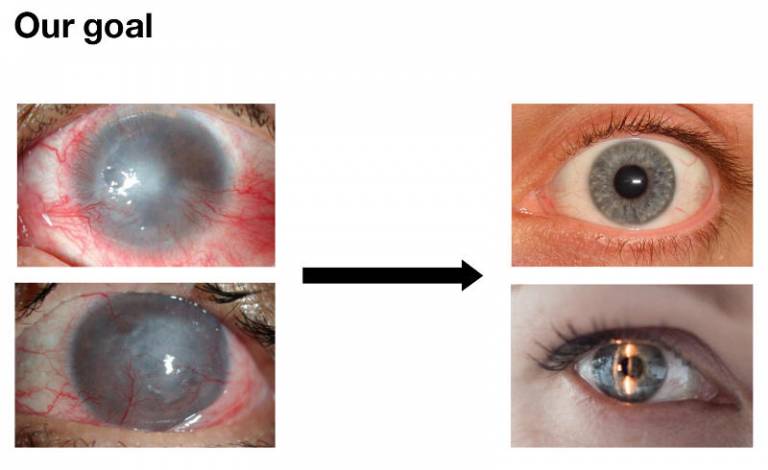
To develop ways of using ‘foreign’ donor corneal stem cells to repair the cornea, and simultaneously prevent the immune system from rejecting these donor cell transplants.
 Close
Close

