Fine-tuning engineered immune cells to improve autoimmunity treatment
18 October 2022
Results from a UCL study point towards a safer and more effective cell therapy that uses genetically engineered regulatory T cells to specifically target and suppress the immune cells that cause autoimmune disease.
Published in the Journal of Autoimmunity, the research results provide a promising basis for clinical trials in patients to explore whether one dose of genetically reprogrammed regulatory T cells can provide long-term protection against autoimmunity without impairing protection against infection and cancer.
Immune system suppressors
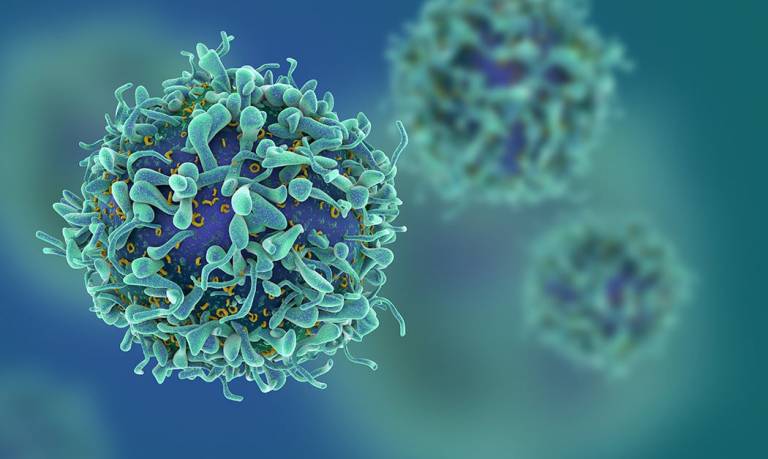
Regulatory T cells (also known as Tregs) are a subset of T cells responsible for the regulation of immune responses. Tregs act by suppressing the immune system and play a critical role in preventing autoimmunity. When Tregs are not functioning properly, the body’s immune system can mistakenly attack healthy tissues and cause autoimmune diseases such as multiple sclerosis, rheumatoid arthritis or type 1 diabetes.
At present, autoimmune conditions are typically treated with drugs that suppress the immune system. And while this approach can be very effective in treating the disease, there are two main drawbacks: patients need to take the drugs daily over a period of many years – often for their lifetime; and the drugs suppress the entire immune system, which makes patients susceptible to infections and, over time, increases the risk of developing cancer.
From drug therapy to engineered cell therapy
“We are looking to see whether we can provide a solution to the drawbacks of current treatment,” says Professor Hans Stauss, Director of UCL’s Institute of Immunity and Transplantation and lead author of the study. “We inserted two genes - TCR and FoxP3 - into regulatory T cells to achieve disease-specific immune suppression, and to ensure that the reprogrammed Tregs retained their suppressive activity over time.
“Our testing in the lab has shown that one intravenous dose of the reprogrammed regulatory T cells resulted in the long-term persistence of the cells that continued to have high levels of the TCR and FoxP3, which are required for disease-specific immune suppression. These results are exciting. The next step would be to test our findings in human clinical trials. If we see in trials what we have seen in the lab, then this therapy has the potential to substantially improve the lives of patients with auto immune diseases.”
Ongoing work at Quell Therapeutics and Apollo Therapeutics is exploiting the reprogramming technology to test its effectiveness in clinical trials.
This work was funded by a pathfinder grant award from the Wellcome Trust.
Further information
- Research paper: Forced Fox-P3 expression can improve the safety and antigen-specific function of engineered regulatory T cells. Journal of Autoimmunity
- Quell Therapeutics
- Apollo Therapeutics
- UCL Institute of Immunity and Transplantation
- Professor Hans Stauss academic profile
 Close
Close

