Fellowship funder:
NIHR Clinical Doctoral Research Fellowship (ICA-CDRF-2017-03-006)
Fellowship outline:
People in prison tend to experience poorer health, poorer access to health care services and poorer health outcomes than people in the general society. The period of incarceration represents a key opportunity for these patients to access relevant health care treatment, given that primary needs such as shelter and food are addressed by the prison environment. However, there are significant barriers associated with prisoners accessing hospital healthcare services and there is an urgent need for research to identify strategies to improve the quality of healthcare for prisoners.
This Fellowship concentrates on patient access to secondary care, defined as health care services and treatment provided by acute hospital sites, using telemedicine, defined as remote video consultations between prison patients and secondary healthcare staff. This research aims to understand the issues involved with implementing prison-hospital telemedicine and to determine whether prison-hospital telemedicine is useable and acceptable to both staff and patients.
 Fellowship holder: Ms Chantal Edge
Fellowship holder: Ms Chantal Edge

This NIHR fellowship was awarded to Chantal Edge in 2018. Chantal is based at UCL for the duration of her fellowship within the Collaborative Centre for Inclusion Health. As a clinical doctoral fellowship she also has a clinical host site for this research, Royal Surrey NHS Foundation Trust, where she maintains a position as an honorary researcher. She also holds an honorary research position with Central North West London NHS Foundation Trust who provide primary care in prisons involved with the research.
Contact details:
Email: c.edge@ucl.ac.uk
Twitter: @ChantalEdge
Background to the research project:
Chantal conceived this research project whilst working clinically on the implementation of prison-hospital telemedicine in Surrey in her role as a Specialty Registrar in Public Health. Following discussions with primary care teams in local prisons she came to realise there were many structural barriers to accessing secondary care from prison, which could potentially be overcome by use of remote video consultation where appropriate. She engaged with the local hospital, Royal Surrey NHS Foundation Trust, who agreed to pilot a telemedicine model with the local prisons and Chantal subsequently led on the development of this intervention. Realising that this was in fact a highly complex change, Chantal applied to NIHR for research funding to collect data on the process of implementation and to evaluate the feasibility of delivering telemedicine appointments to prisons.
Fellowship supervisors:
- Professor Andrew Hayward (Primary Supervisor)
- Dr Georgia Black (Secondary Supervisor)
- Dr Julie George
- Dr Rachael Hunter
- Professor Aftab Ala (Clinical Supervisor Royal Surrey NHS Foundation Trust)
- Dr Simon Edwards (Clinical Supervisor Central North West London NHS Foundation Trust)
- Dr Shamir Patel (Principle Investigator – Central North West London NHS Foundation Trust)
- Dr Michelle Gallagher (Principle Investigator – Royal Surrey NHS Foundation Trust)
Project partners:
- The Prison Reform Trust
- Royal Surrey NHS Foundation Trust
- Central North West London NHS Foundation Trust, Offender Care Team
Ethics approvals:
This research has received approvals from the South East London NHS Research Ethics Committee (19/LO/0098), the HMPPS National Research Committee (NRC-186) and the Health Research Authority (IRAS 229646). The study is also adopted to the Clinical Research Network Portfolio (CPMS ID [37625]). This study is sponsored by the UCL Joint Research Office.
Research methods outline:
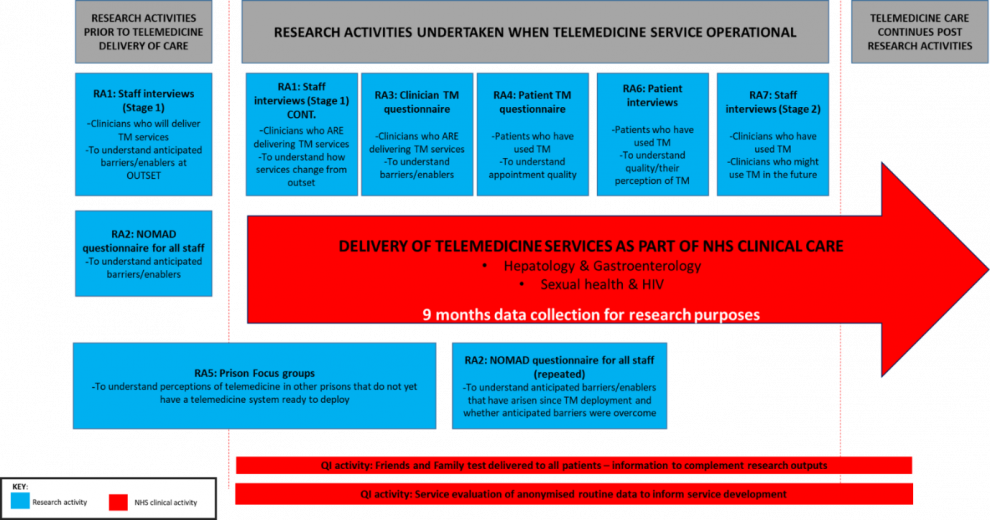
Pre-implementation Research Activities (RAs)
RA1: Staff Interviews (Stage 1)
We will conduct a series of 1:1 semi-structured interviews (maximum n=30) amongst telemedicine stakeholders from all staff groups. Through interviews we will seek to understand anticipated benefits, barriers and enablers to telemedicine usage in a prison-hospital setting, within the English commissioning context. The interview guide has been developed based on the NPT constructs.
RA2: NOMAD questionnaire
The NOMAD questionnaire is an existing validated questionnaire, based on the principles of normalisation process theory (Finch et al., 2018). The NOMAD questionnaire seeks to identify barriers to normalisation of an intervention in healthcare to explain why interventions fail to embed in day to day use. We will administer this anonymous email survey questionnaire to all healthcare staff and additionally to prison officers at participating prisons. This will collect data on staff perceptions and concerns surrounding telemedicine. This questionnaire will be administered prior to telemedicine implementation and several months after implementation, and the changes in response quantified.
RA5: Prison Focus Groups
Study prisons have been advocating for telemedicine introduction for several years and prisoners are aware it may soon be introduced. We will collect data to represent broader prisoner views on telemedicine in prison focus groups (n=5) where there is currently no ‘threat’ of implementation and prisoners will be free to speak openly of their concerns. Results will be used where applicable to inform the current telemedicine service implementation and to inform policy for future telemedicine services if research results suggest it can be widely implemented. For example: “What do you think would stop people wanting to use a telemedicine system and how could we mitigate this?” The topic guide for focus groups will be guided by the TFA.
Implementation Research Activities
These activities will commence after telemedicine has become operational in at least one prison site.
RA1: Staff Interviews (Stage 1) continued
Frontline delivery staff will be re-interviewed during implementation to understand how the telemedicine services proposed at outset have changed and adapted as issues arise, and what specific barriers have arisen that were not anticipated.
RA3: Clinician questionnaire on telemedicine appointment
Both hospital clinicians and prison healthcare staff involved in a telemedicine appointment will complete a short paper questionnaire at the close of each appointment. This will seek to understand whether the appointment was clinically acceptable, with reference to anticipated barriers identified in the staff interviews at outset.
RA4: Patient questionnaire on telemedicine appointment
All patients who have a telemedicine appointment will be offered a short, anonymous paper questionnaire immediately after their appointment finishes, to collect data on patient acceptability of telemedicine appointments. Questionnaires should provide information that may be overlooked as ‘not important’ or not recalled in later patient interviews e.g. “Did the doctor speak over you?”, “Could you hear the doctor clearly?”.
The content of the questionnaire will be based on the Telemedicine Usability Questionnaire (TUQ) with several additional questions pertaining to appointments in prison. For example, “Were you able to get to your appointment on time?” which refers to the fact that prison officers will need to escort patients to their telemedicine appointment within the prison healthcare department.
The questionnaire will be finalised with input from a PPI (patient public involvement) group convened inside the prison to ensure the questionnaire is comprehensible and relevant to people in prison.
RA6: Patient 1:1 interviews
1:1 semi-structured interviews (n=15) will be held with patients who have had a telemedicine consultation to collect information on patient experience and acceptability. Where applicable participants will be asked to compare telemedicine treatment to previous offsite secondary care appointments.
RA7: Staff interviews (stage 2)
Interviews with staff who have used the telemedicine system with seek to understand the feasibility and acceptability of the current delivery model. Interview topic guides will be informed by NPT constructs and results of the NOMAD survey previously administered.
Quality Improvement (QI) Measures
The NHS Friends and Family Test
Alongside the research activities a standard NHS QI tool (the Friends and Family test) will be administered by the prison healthcare staff to patients, to monitor satisfaction of telemedicine services for all appointments. Anonymised data from this will be provided to the research team to supplement the research summary and will be compared to pre-telemedicine satisfaction scores.
Quantitative Service Evaluation - Pre and Post Anonymised Health Records Data for Specialties under Study
After nine months of service delivery routine service evaluation data will be used to assess clinical effectiveness, specifically to understand whether appointments happened more quickly using telemedicine and whether cancellations were reduced. This data will be compared at stages throughout implementation to pre-telemedicine data on the same indicators, to account for a transition phase as the service becomes established.
Service Evaluation to Inform Wider Specialties for Telemedicine Delivery
This analysis will help inform which other hospital specialties may be areas of value for telemedicine development e.g. department with most referrals, department with longest wait, department with most cancellations. This will complement stage 2 staff interviews on wider telemedicine specialties.
Economic analysis
Cost modelling will be undertaken by a health economist to understand how the wider rollout of prison telemedicine across specialties may affect cost effectiveness of secondary care delivery to prisoners (including costs to prison healthcare provider, wider prison costs and NHS costs).
Patient and Public Involvement (PPI) Plans:
Chantal is working with the Prison Reform Trust to involve current prisoners in the design of this research. PPI groups have been run in one male and one female prison in Surrey to input into patient questionnaire design, focus group topic guides and mythbusting information around telemedicine appointments. These groups will be convened throughout the research to input on other aspects of the study or interpretation of the results.
Chantal also has two PPI advisors based in the community who have lived experience of imprisonment. These advisors attend meetings and helped design materials for submission to ethical committees.
The graphic design workshop at HMP Coldingley (staffed by current prisoners) is working with Chantal to design all the materials for telemedicine advertising campaigns within prisons.
Progress to date:
Research
Chantal has received all relevant ethical approvals for her research and completed and published a systematic review on barriers and facilitators to prison telemedicine. She has also completed a qualitative analysis project (see other research) to understand the issues prisoners face with accessing secondary care in the current (non-telemedicine) system of appointments.
Chantal also visited the University of Texas Medical Branch, Department of Correctional Managed Care in 2018, to learn about their successful prison telemedicine service that has been running since the 1990s.

Picture: UTMB Correctional Managed Care Team visit, Texas
Chantal is now undertaking a series of pre-implementation interviews with staff from hospital and prison healthcare teams to understand problems to date and future concerns regarding telemedicine implementation (Research Activity 1), and planning delivery of focus groups in prisons (Research Activity 5).
Clinical
The proposed telemedicine system in study prisons has just been approved for use by the central HMPPS IT Management and Security Team, making this the first approved service in England. The videoconferencing software to be used is Visionable.
A template SysOPs will be available for distribution by early 2020, following minor amendment in line with HMPPS requirements.
The main hospital and prison site involved in this pilot are happy to take requests from other prisons/hospitals who wish to see this intervention. Please contact c.edge@ucl.ac.uk in the first instance if you wish to be put in touch.
Published papers relating to this fellowship:
Reports and documents freely available:
Coming soon…
- SysOPs (operational protocol document) for Visionable use for prison telemedicine. The SysOPs document for Visionable use for prison telemedicine systems has been completed and approved by HMPPS. To request a copy of this document for use in establishment of your own prison-hospital telemedicine model please email c.edge@ucl.ac.uk
- These posters can be edited in any graphics software program. These posters were designed by Mark Alexander at HMP Coldingley. If you would like the prison to undertake any design work or printing please contact jane.ashwood@justice.gov.uk
- Patient prison telemedicine questionnaire
- Clinician prison telemedicine questionnaire
Media outputs:
- Blog - Inclusion Health: Co-producing a research and advocacy agenda | UCL Institute of Epidemiology and Health Care Blog
- Podcast -9 July 2019 - We Remember Lives – The Hospice Biographers Episode 10
Conference presentations:
- HSRUK Conference June 2019 - Using Animation To Capture The Healthcare Experiences Of People In Prison
- Upcoming - Health and Justice Summit Nov 2019 – Systems barriers to prison telemedicine in England
Posters:
Presented at both the NIHR Academy Conference November 2018 and UCL postgraduate poster competition 2018.
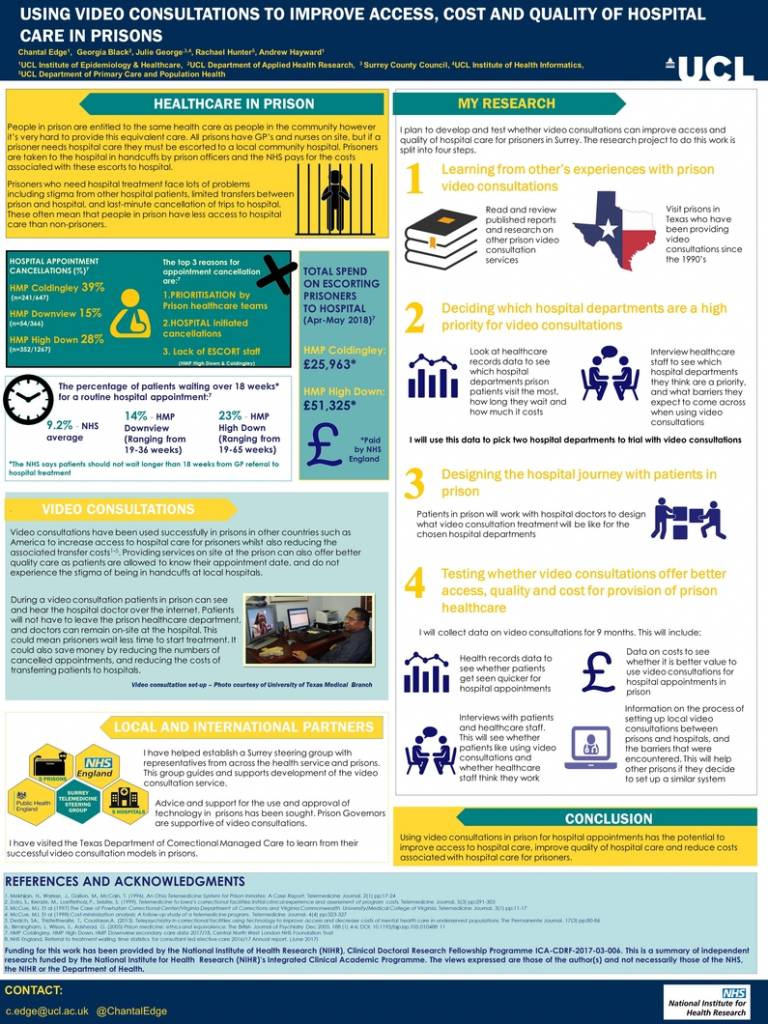
Associated awards:
- NIHR Academy Conference November 2018 – Poster award
- UCL postgraduate poster competition 2018 – Runner up poster award
- HSRUK Conference 2019 – Runner up best presentation award
Other research projects:
Chantal is also the Chief Investigator on a jointly funded Wellcome Trust & Surrey Heartlands Health and Care Partnership research project entitled:
“Using animation to capture the healthcare experiences of people in prison”.
This project brought together a diverse group of project partners to create an animation based on patient experiences of accessing hospital care from prison. This animation will be tested to see if it influences community health professionals to think of ways they can deliver better quality care to patients from prison, for example, through development of telemedicine services.
 Close
Close

