Microbial Diseases
Our research in this area falls into two categories:
Antimicrobial resistance and novel antimicrobial therapies
Antimicrobial resistance is a global threat and there is an urgent need to develop new antimicrobials and novel antimicrobial strategies. The objectives are to understand the evolution of antimicrobial resistance and to develop novel antimicrobial therapies. This work is led by a group of researchers who are internationally recognised for the development of photodynamic therapy to treat microbial diseases.
Biofilms and the Microbiome
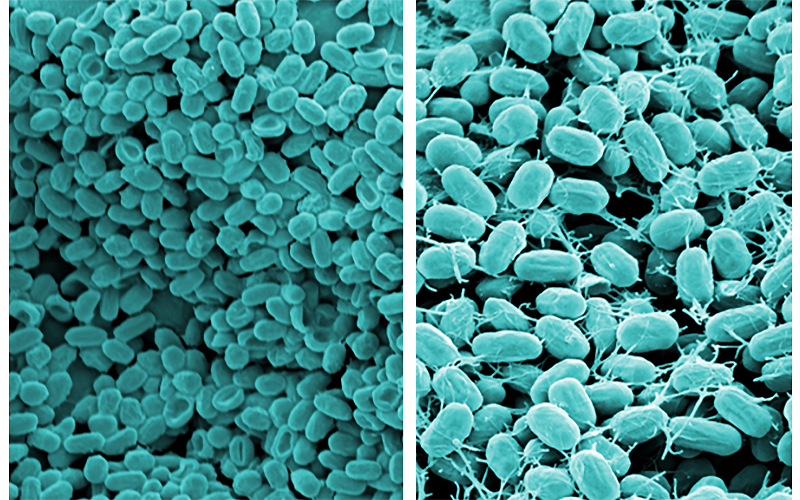
Biofilms are responsible for around 80% of all infections, in addition to being found naturally in the environment and co-existing with humans in the form of our indigenous microbiota. UCL Eastman is internationally regarded as one of the pioneer centres for biofilm research focusing on oral bacteria and bacteria associated with healthcare infections. Active research programmes associated with this theme are investigating the composition of biofilms, their mechanisms of formation, their resistance to antimicrobials, the development of novel anti-biofilm therapies and novel therapies based on modulation of the microbiota.
- Meet our researchers
Dr Sean Nair PhD BSc Hons.
Reader and Head of Microbial DiseaseAreas of interest: (i) Interactions of bacteria with host cells. Focusing on the mechanisms by which Superbugs (e.g. staphylococci/MRSA, and enterococci/VRE) cause disease. (ii) Development of novel antimicrobial strategies to combat infections. The use of antisense/aptamer technologies, development of light-activated antimicrobial agents and identification of bacterial genes coding for potential novel therapeutic targets. Find out more
Recent paper: Liu C, Zhou Y, Wang L, Han L, Lei J, Ishaq HM, Nair SP, Xu J. (2016) Photodynamic inactivation of Klebsiella pneumoniae biofilms and planktonic cells by 5-aminolevulinic acid and 5-aminolevulinic acid methyl ester. Lasers Med Sci. 2016 Feb 17. DOI: 10.1007/s10103-016-1891-1016-1891-1.
Dr Elaine Allan BSc (Hons), PhD
Senior Lecturer in Molecular MicrobiologyAreas of interest: Molecular basis of bacterial virulence, Environmental signal transduction, Biofilm formation, exopolymeric matrix composition and regulation, Metagenomics for natural product discovery, New antibacterial approaches. Find out more
Recent paper: Waheed Jowiya, Haitham A. Hussain, Sean P. Nair, Sohaib Sadiq, Lisa K. Williams, Emma K. Trantham, Holly Stephenson, Brendan W. Wren, Mona Bajaj-Elliott, Tristan A. Cogan, Andrew P. Laws, Jim Wade, Nick Dorrell, Elaine Allan. 2015. Pancreatic amylase is an environmental signal for regulation of biofilm formation and host interaction in Campylobacter jejuni. Infect. Immun. 83:4884-95.
Dr Dimitrios Evangelopoulos, BSc, PhD
Lecturer in MicrobiologyAreas of interest: I am interested in the discovery and identification of new therapeutics and interventions towards bacterial diseases. I am investigating the molecular and cellular mechanisms of antibiotic action and resistance in bacteria. Additionally, I am very interested in exploring the fundamental biology of bacterial vitamin biosynthesis pathways and understanding their role during pathogenesis. Find out more
Recent paper: Dimitrios Evangelopoulos, Gareth A. Prosser, Angela Rodgers, Belinda M. Dagg, Bhagwati Khatri, Mei Mei Ho, Maximiliano G. Gutierrez, Teresa Cortes & Luiz Pedro S. de Carvalho. Comparative fitness analysis of D-cycloserine resistant mutants reveals both fitness-neutral and high-fitness cost genotypes. Nat Commun. 2019; 10: 4177.
Prof Peter Mullany BSc, PhD
Professor Microbial DiseasesAreas of interest: Transfer of genes between bacteria; including the transfer of antibiotic resistance genes. The molecular biology of the important human pathogen Clostridium difficile. Find out more
Recent paper: Arivaradarajan P, Warburton PJ, Paramasamy G, Nair SP, Allan E, Mullany P. Identification of an antibacterial protein by functional screening of a human oral metagenomic library. FEMS Microbiol Lett. 2016 Jan;363(1).
Prof Andrew Mark Smith BSc (Hons), PhD,
Chair in Oral Health SciencesAreas of interest: Andrew Smith’s research is focused on understanding the innate immune response within healthy and diseased tissue. He has ongoing collaborative projects investigating the role the innate immune system plays in Crohn’s disease, ulcerative colitis, orofacial granulomatosis, lichen planus and mucosal inflammation. Find out more
Recent paper: O'Loughlin T, Kruppa AJ, Ribeiro ALR, Edgar JR, Ghannam A, Smith AM, Buss F. OPTN recruitment to a Golgi-proximal compartment regulates immune signalling and cytokine secretion. J Cell Sci. 2020 Jun 15;133(12):jcs239822. doi: 10.1242/jcs.239822.
Dr Gregory Sebepos-Rogers BSc MBBS MRCP MSc
Crohn’s & Colitis UK Clinical Research FellowAreas of interest: I am interested in better understanding the molecular mechanisms driving disease causation and progression in Inflammatory Bowel Disease. My current area of focus is innate immunity and the role of Optineurin, a widely found cell-based molecule previously characterised by my supervisor Prof Smith. During my PhD, I will investigate how this molecule influences key inflammation pathways in relation to Crohn’s disease. Find out more
Recent paper: Gadhok R, Gordon H, Sebepos-Rogers G, Baillie S, Akbar S, Abbott JE, Michael E, Ahmad OF, Cooper B, Lindsay JO. UK Patients of Bangladeshi Descent with Crohn's Disease Respond Less Well to TNF Antagonists Than Caucasian Patients. Dig Dis Sci. 2019
Prof David Spratt BSc, PhD
Professor of Microbial Ecology and Education,
Head of EducationAreas of Interest: Human microbial communities in health and disease, modelling biofilms to understand microbial ecology, biofilms associated with failed implants. Find out more
Recent paper: Sousa V, Nibali L, Spratt D, Dopico J, Mardas N, Petrie A, Donos N. Peri-implant and periodontal microbiome diversity in aggressive periodontitis patients: a pilot study. Clin Oral Implants Res. 2016 May 11. doi: 10.1111/clr.12834.
- Facilities
Microbial Diseases has state-of-the-art laboratories for bacterial and genetic modification work that contain class I and class II biological safety cabinets and anaerobic chambers. There are large cold rooms for protein purification work and warm rooms for aerobic bacterial culture, and dedicated laboratories for microscopy (light and fluorescent), molecular biology (sample preparation robot, PCR and QPCR machines), mammalian tissue culture work, and biofilm work (apparatus for fermentation and for numerous biofilm models.
- All current PhD projects
1. Antibiotic resistance and the development of novel antimicrobial therapies
Project titles:
- Macrolide resistance in the oral cavity: mechanisms and transfer Supervisor: Dr Elaine Allan
- Signal transduction in bacterial virulence Supervisor: Dr Elaine Allan
- Identification of novel therapeutic targets in bacteria associated with healthcare infections such as Staphylococcus aureus and 'superbugs': Staphylococcus aureus, MRSA, enterococcus, VRE, virulence Supervisor: Dr Sean Nair
- Development of novel antimicrobial agents and identification of antimicrobial agents produced by microorganisms: novel antimicrobials, metagenomics, antimicrobial peptides, bacteriocins Supervisor: Dr Sean Nair
- Targeted photodynamic therapy for bacterial infections photosensitizers, singlet oxygen, targeting molecules, MRSA, staphylococcus Supervisor: Dr Sean Nair
- Novel approaches to understanding how the important nosocomial pathogen Clostridium difficile causes disease: Clostridium difficile, virulence, antimicrobial associated disease Supervisor: Dr Peter Mullany
- A synthetic biology approach to the development of phage therapy to bacterial diseases phage: oral microbiota, caries Supervisors: Dr Peter Mullany / Dr Susan Parekh / Dr Paul Ashley
- Exploring gene transfer in the whole oral microbiota: metagenomics, oral microbiota, mobile genetic elements Supervisor: Dr Peter Mullany
- Identification of natural antimicrobial agents for the treatment of periodontal diseases: periodontal pathogens, natural antimicrobials Supervisor: Dr Sean Nair
- New therapeutics for tuberculosis: identification and characterisation of cofactor biosynthesis pathways and their role during infection Dr Dimitrios Evangelopoulos
- Rational design of future drug combinations as a strategy to combat antibiotic resistance and superbugs Dr Dimitrios Evangelopoulos
2. Biofilms and the microbiomeProject titles:
- Biofilm disruption activities in natural environments Supervisor: Dr Elaine Allan
- Metagenomics for natural product discovery Supervisor: Dr Elaine Allan
- Development of new strategies for treating implant infections: biofilms, enterococci, periodontal pathogens, Staphylococcus aureus, Staphylococcus epidermidis Supervisor: Dr Sean Nair
- Molecular mechanisms of biofilm formation: Staphylococcus aureus, MRSA, VRE Supervisor: Dr Sean Nair
- Synthetic biology to develop agents for disrupting medically important biofilms: molecular breeding, domain shuffling, enzymes Supervisor: Dr Sean Nair
- Understanding biofilm regulation in Campylobacter jejuni: biofilms, signalling, virulence Supervisor: Dr Elaine Allan
- Constant depth film fermentor models of gingivitis and periodontitis: gingivitis, periodontitis, biofilms Supervisor: Professor David Spratt
- Mucosal immune response in health and disease innate: adaptive, immunity, inflammation, macrophage, Toll-like receptors Supervisor: Dr Andrew Smith
- Transcriptomic analysis of oral inflammatory disease: transcriptomics, inflammation, human disease, next generation sequencing, bioinformatics Supervisor: Dr Andrew Smith
- The human microbiome in health and Disease: metagenomics, functional metagenomics, host-microbe interactions. Supervisors: Dr Sean Nair, Professor David Spratt
- Bacterial vitamin biosynthesis pathways and their role in the homeostasis of the oral microbiome Dr Dimitrios Evangelopoulos
 Close
Close