Defining the contribution of B cell immunopathology to the development of juvenile idiopathic associated uveitis.
Primary Supervisor: Prof Lucy Wedderburn
Secondary Supervisor: Dr Elizabeth C. Rosser
Hypothesis and/or Aims:
In this project, the student will test the hypothesis that uveitis development in patients with Juvenile Idiopathic Arthritis (JIA) is driven by B-cell dysfunction. This will be addressed by answering the following research aims.
AIM 1: Identify a uveitis-specific B-cell immunological fingerprint in JIA-patients.
AIM 2: Interrogate mechanistic targets underlying B-cell dysfunction in JIA-uveitis patients.
AIM 3: Assess the role of B-cell-driven immunopathology in experimental autoimmune uveitis.
6-12 month plan (eg experimental approaches, data collection, preliminary analyses):
In the first period of the project, the student will be trained in flow cytometry, large data-set handling (clinical outcome data and RNAseq) and animal handling. Alongside training, the student will stratify the large JIA-patient cohort data generated by the CLUSTER consortium (peripheral blood mononuclear cells, PBMC, from ~150 patients and paired PBMC and synovial fluid mononuclear cell samples, SFMC, from 47 patients – majority collected pre-DMARD/biologics) including basic immune-phenotype by flow cytometry (CD4+T-cells, CD8+T-cells, CD19+B-cells, CD14+monocyte subsets), transcriptional data on bulk sorted subsets (CD4+T-cells, CD8+T cells, CD19+B-cells, CD14+monocytes), genotype, proteome, and integrated longitudinal clinical data, by JIA-uveitis phenotype e.g. uveitis-ever versus uveitis-never (as defined at 3 year follow-up); initial screening suggests that 15-20% of this data-set falls within the ‘uveitis-ever’ patient group. Using these data, gross B-cell subset frequency (CD19+CD24hiCD38lomemory B-cells, CD19+CD24intCD38intmature naïve B-cells, CD19+CD24hiCD38hiimmature B-cells, CD19+CD24loCD38hiplasmablasts and CD19+CD24loCD38hiatypical memory B-cells) and transcriptional differences in sorted CD19+B-cells between a large group of uveitis-ever versus uveitis-never JIA patients will be assessed. Where possible, linear regression models will be used to integrate disease covariates (age of onset, disease activity) with immunological data. As well as analysis of differentially expressed genes (DEG), gene-set enrichment, pathway and network analysis (DAVID, KEGG, REACTOME) will be carried out upon CD19+ transcriptional data. These analyses will identify whether DEG are associated with particular pathological changes to biological and functional pathways in JIA-uveitis CD19+B-cells.
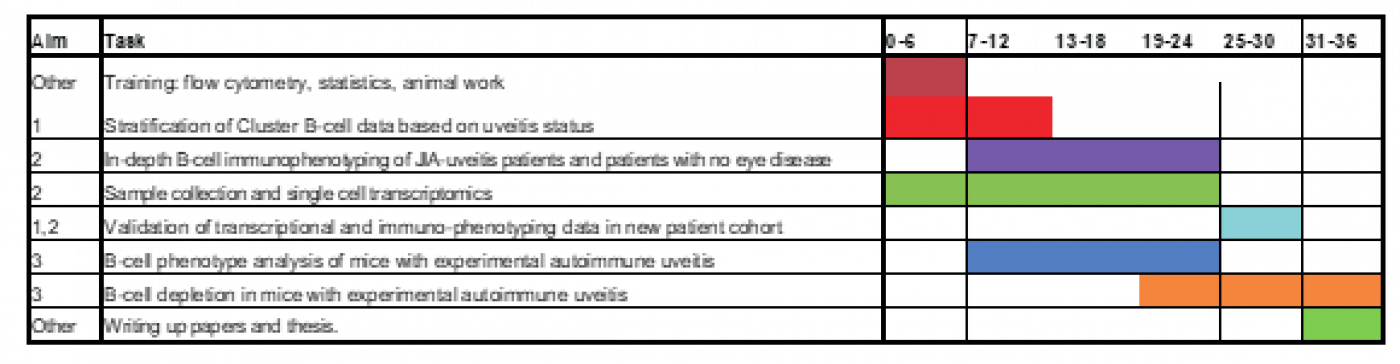
Timeline:
Ethics Approval (if applicable): approval already in place for all parts of the work
Human Ethics: 95RU04 (IRAS ref 207607), Bloomsbury REC
Animal Ethics: PP3383641
References (max. 5):
1 Petty, R. E. & Zheng, Q. Uveitis in juvenile idiopathic arthritis. World J Pediatr, doi:10.1007/s12519-019-00331-6 (2020).
2 Cumberland, P. M., Rahi, J. S., Eye, U. K. B. & Vision, C. Visual Function, Social Position, and Health and Life Chances: The UK Biobank Study. JAMA Ophthalmol 134, 959-966, doi:10.1001/jamaophthalmol.2016.1778 (2016).
3 Qian, Y. & Acharya, N. R. Juvenile idiopathic arthritis-associated uveitis. Curr Opin Ophthalmol 21, 468-472, doi:10.1097/ICU.0b013e32833eab83 (2010).
4 Wilkinson, M. G. L. & Rosser, E. C. B Cells as a Therapeutic Target in Paediatric Rheumatic Disease. Front Immunol 10, 214, doi:10.3389/fimmu.2019.00214 (2019).
 Close
Close

