UCL Medicine-Chemistry collaboration breaks new ground for Diagnostic Imaging
13 September 2017
A University College Hospital patient has been diagnosed with prostate cancer using a hyperpolarised MRI scan in August this year, as part of a UCL trial looking to develop more accurate and personalised treatment for cancer. The scan was the first time this experimental imaging method was used in Europe to scan a patient with prostate cancer and was able to help doctors confirm the location and state of the patient’s tumour. The trial, led by Dr Shonit Punwani, is a novel programme hoping to revolutionise diagnosis, risk stratification and therapy for people with cancer, based on innovations in MRI technology.
Hyperpolarised MRI is an emerging medical imaging technique that uses carbon-13 enriched metabolites as tracers, in particular 13C-pyruvate. Hyperpolarisation with dynamic nuclear polarization give a signal increase 10,000 times above conventional NMR. This allows the metabolic activity of tumours, such as transformation of pyruvate to lactate, to be measured in patients. The goal of the study is to determine if metabolic information, along with anatomical imaging, can allow more accurate diagnosis and stratify patients for treatment. However, the technology is still at an early stage and depends on extensive collaboration between medical sciences and Chemistry.
The GMP team; Frazer Twyman, Matthias Glaser, Ramla Awais, Thibault Gendron, Erik Arstad (Chemistry) and Kerstin Sander (Chemistry).
The Good Manufacturing Practice (GMP) facility, led by Prof Erik Arstad (Chemistry), played a central role in this study by developing a process for filling of kits with 13C-pyruvate under sterile conditions. Advances made at UCL allowed for the first time to fill such kits in a laminar air flow isolator, an important step towards formal trials with hyperpolarised MRI in patients. Following filling, the kits are pressured with helium to allow for the extreme conditions needed to hyperpolarise the tracer, and the whole assemble is finally laser-welded in a clean room.
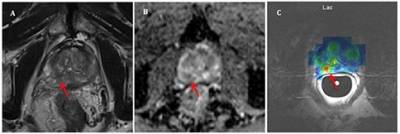
These three images show an axial T2 weighted MRI (Image A) and Apparent Diffusion Coefficient map (Image B) acquired as part of a routine multi-parametric MRI study of the prostate. 13C spectroscopic lactate image (Image C) demonstrates high levels of lactate at the position of the biopsy positive Gleason 3+4 tumour site (red arrow).
Dr Shonit Punwani, Reader in Magnetic Resonance and Cancer Imaging and UCLH honorary consultant radiologist, said: “The multi-disciplinary research team have spent the past two years installing and testing the equipment, creating standard operating procedures and planning the study in great detail. We are really pleased to have scanned our first patient and we will continue to work closely with other sites, in the UK and internationally, to develop this technology further.” Dr Punwani is the principal investigator of the Hyperpolarised MRI study which is developing the technology so that a full clinical evaluation can take place.
Prof Erik Arstad, Director of the GMP facility, said: “This is a major achievement following extensive work to allow filling of kits for hyperpolarised MRI under sterile conditions, and to ensure efficient and safe hyperpolarisation prior to patient scanning. With the first patient scan on Campus, the work has open up for a number of diagnostic studies that can help advance hyperpolarised NMR to become a routine clinical tool”.
The equipment underpinning this work is a new Spinlab Hyperpolariser from GE situated at the University College Hospital Macmillan Cancer Centre, and designed to work in conjunction with existing MRI equipment to provide non-invasive metabolic assessment of tumours. The study is supported by funding from the Medical Research Council, the Wellcome Trust, the National Institute of Health Research UCLH Biomedical Research Centre (where Dr Punwani is Director of Clinical Imaging), Cancer Research UK, as well as philanthropic funding from the Mitchell Charitable Trust.
 Close
Close

