Transforming the lives of children with severe epilepsy
Clinical scientists at UCL have devised a new care pathway for children with severe epilepsy, incorporating state-of-the-art imaging and machine learning tools, which is transforming patients’ lives.
28 April 2022
Approximately 35,000 children and young people in the UK experience severe uncontrolled epilepsy that is associated with a reduced quality of life.
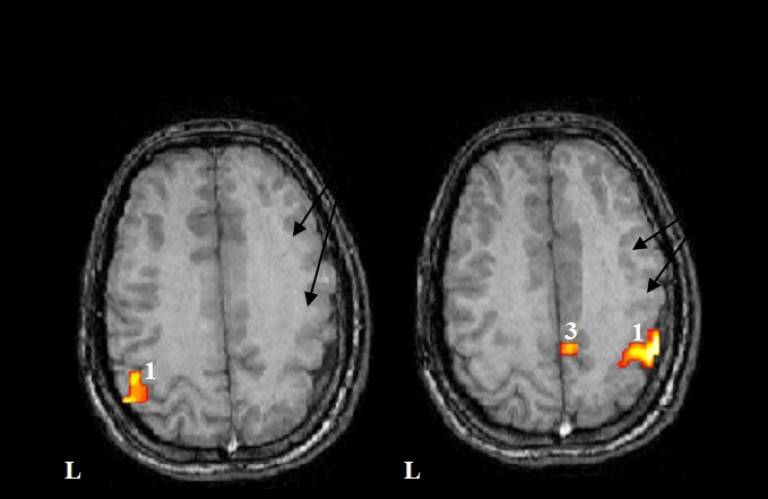
Professors Helen Cross and Torsten Baldeweg, clinical scientists at UCL Great Ormond Street Institute of Child Health (GOS ICH), led developments in MRI scanning to pinpoint the problem areas in the brain that cause seizures.
Their research also highlighted the value in increasing epilepsy surgery as an intervention for severe epilepsy, demonstrating that early surgery and subsequent weaning from medication can arrest cognitive decline. They estimate that up to 440 children per year in England can benefit.
The care pathway developed by the UCL team is now included as standard-of-care in international guidelines. The MRI brain scans help clinicians to identify children who will benefit from surgery which reduces epileptic seizures and can help educational development.
Helping more children get the care they need
To ensure children who could benefit from surgery are identified and treated, Professor Cross established the Children’s Epilepsy Surgery Service (CESS) – a centralized epilepsy surgery service for children in England.
In 2019, 345 children in England had the surgery (a three-fold increase since 2013). Eight out of ten of these children have stopped having seizures. Many have also stopped taking epilepsy medication, which has arrested a progressive decline in IQ and educational attainment.
To identify more patients suitable for epilepsy surgery who would have been missed using standard clinical evaluation, the UCL team initiated a multi-centre effort to catalogue brain scans and develop a large training data set - the ‘Multi-centre Epilepsy Lesion Detection’ (MELD) project.
Participating centres use their own scan data for clinical planning and then, using software tools developed at UCL, compare it to data from collaborating centres. Scan data from the collaborating centres is used to further develop the tools for lesion detection and normalisation techniques through machine learning.
Creating an international network of best practice
The MELD cohort currently comprises over 550 patients with Focal Cortical Dysplasia (FCD; a marker of epilepsy) and 382 controls, with 26 participating centres internationally, including in Brazil, China, Finland, Spain and US.
To support wide access to high quality care, the UCL team led the development of the pilot Reference Network for Epilepsy Surgery (E-pilepsy), and subsequently established the Network for Rare and Complex Epilepsies (EpiCARE,) of which ‘E-pilepsy’ remains the surgical arm. This is now a network of 38 specialist health care centres and a further 13 affiliated centres across 24 countries who work together to provide specialist advice on treatments for complex epilepsy cases.
Research synopsis
Widening access to curative surgery for children with refractory focal epilepsy
State of the art imaging and a new care pathway devised by clinical scientists at UCL are transforming the lives of hundreds of children with severe epilepsy. The team has built international clinical networks and developed machine learning tools that help ensure children suitable for curative surgery can benefit.
Links
- Professor Helen Cross’ academic profile
- Professor Torsten Baldeweg’s academic profile
- UCL Great Ormond Street Institute of Child Health
- UCL Faculty of Population Health Sciences
- UCL Population Health Sciences REF 2021
Image
- Image credit: Torsten Baldeweg
 Close
Close

