Enabling safer, better and quicker pre-natal testing
Genetic tests developed at UCL Great Ormond Street Institute of Child Health (UCL GOS ICH) have transformed care for families at risk of genetic diseases.
27 April 2022
When families want to know if their unborn baby has a genetic condition, because a parent is a carrier or they have a previous child with this serious genetic condition, clinicians need to test the baby’s genetic material - their DNA. This is usually done by putting a needle into the womb to sample the placenta (chorionic villus sampling) or amniotic fluid (amniocentesis) - both have a small miscarriage risk.
As a baby’s DNA is present in their mother’s blood from early pregnancy, UCL researchers were among the first to develop maternal blood tests to detect genetic abnormalities in unborn babies by analysing this DNA in mothers’ blood. They helped the clinical laboratory establish the first accredited non-invasive prenatal diagnosis (NIPD) service for genetic conditions world-wide. NIPD results are available within five days, earlier than standard invasive testing.
Initially these tests were limited to conditions the team knew were not inherited from the mother. This is because if she does not carry the faulty gene and it is detected in the test, it must therefore belong to the baby.
Identifying recessive conditions
A team of UCL researchers led by Professor Lyn Chitty (UCL GOS ICH) have now developed NIPD tests for conditions where the baby needs to inherit the genetic abnormality from both parents – these are known as recessive conditions. In these situations, the mother’s faulty gene also circulates in the blood so the team uses highly sensitive counting methods to compare the amounts of the faulty gene to regular gene – this is higher if the baby carries two copies of the faulty gene.
The researchers have also developed ‘bespoke’ testing for around 250 families with very rare conditions where a sibling or the father has the gene.
Parents have welcomed this safer testing as numbers seeking testing have increased tenfold annually (2 vs 20) for cystic fibrosis, as parents can find out about their baby’s health without the invasive test risks. At Great Ormond Street Hospital (GOSH), the team have done more than 2,100 NIPDs for nearly 2,000 families and 190 conditions, and are exploring new methods to expand the NIPD service to more conditions such as sickle cell anaemia.
NIPD is now included in the NHS National Genomic Test Directory, so all families can access it, with GOSH and Birmingham Women and Children’s Hospital hosting the two laboratories for this national service. As most countries do not offer NIPD for genetic conditions, the team also take referrals from around the world.
Speeding up results
Unborn babies with malformations found on ultrasound often have rare genetic conditions. It can take years and multiple tests to make the diagnosis, which delays treatment and is too slow for use in pregnancy.
UCL GOS ICH researchers have developed new methods to rapidly examine DNA from parents and their unborn baby (‘trio exome sequencing’) with results in two weeks. Working with partners on a nationwide study, the team identified which problems in unborn babies were most likely to be genetic, e.g. multiple malformations, or skeletal problems were most likely to be genetic. Their studies helped NHS England include rapid genomic sequencing in the National Genomic Test Directory, so everyone in England can access these tests if needed.
In the first 15 months, rapid sequencing for unborn babies, delivered from GOSH and Birmingham Women and Children’s Hospital, made a diagnosis in 35% of cases tested in an average of 14 days, allowing parents to make informed decisions about the pregnancy.
Throughout the research, the team seek families’ and health professionals’ perspectives to ensure tests meet their needs, with parent advocates included as co-applicants on grants and advising on interacting with parents in these difficult circumstances.
Research Synopsis
Safer, better, quicker pre-natal testing
Genetic tests developed at UCL GOS ICH have transformed care for families at risk of genetic diseases. The tests include non-invasive prenatal diagnosis (NIPD) during pregnancy and rapid exome sequencing to diagnose genetic conditions in at-risk children before they are born.
Links
- Professor Lyn Chitty’s academic profile
- UCL Great Ormond Street Institute of Child Health
- Faculty of Population Health Sciences
- Faculty of Population Health Sciences REF 2021
Image
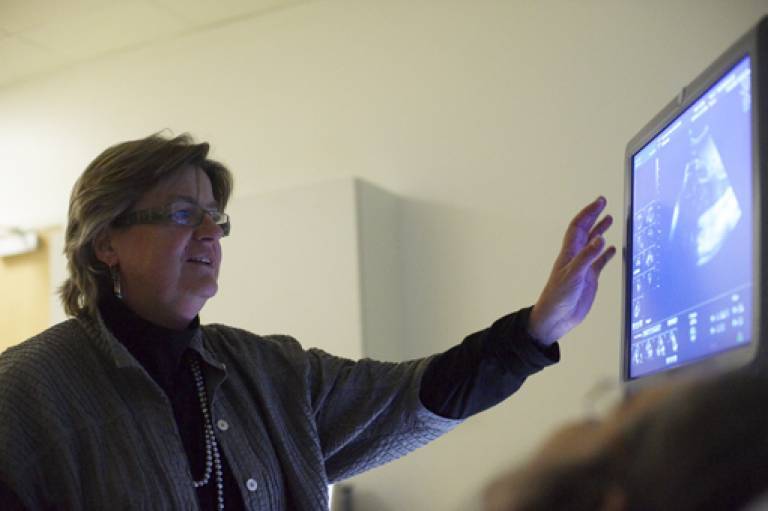
- Image credit: Professor Chitty
 Close
Close

