Research Aims
T cells naturally protect us from infections but they can be diverted to kill cancer cells through gene-engineering. A Chimeric Antigen Receptor (CAR) is a synthetic recognition molecule which can be introduced into T cells and confers an ability to potently recognise cancer cells. Once they recognise a cancer cell, CAR T cells are activated to kill the cancerous cells as well as multiply. They expand in number as they mount a fight against even advanced forms of cancer. At later time points, they naturally contract in number but can persist for years at a low level, forming immunological memory which can continue to protect a patient from relapse. This is similar to a long-lived vaccine response. CAR T cell therapy has been very successful in treating some forms of leukaemia (particularly acute lymphoblastic leukaemia in children) and lymphoma, even when other therapies including chemotherapy and bone marrow transplantation have failed.
Whilst effective in Acute Lymphoblastic Leukaemia (ALL), currently about half of patients treated with CAR T cells are cured, and at least half relapse. This is either because the CAR T cells don’t persist long term or because the cancer cells evolve to escape recognition. CAR T cell therapy can be toxic because of the extreme activation of the immune system that can happen. Together with Persis Amrolia and Martin Pule, we pioneered a novel form of CAR T cell therapy which seems less toxic. The CAR T cells persist long term in most patients.
We have a long way to go in terms of fully understanding what makes CAR T cell therapy effective in some cases. We don’t know why in some cases, CAR T cells only persist for a short time and why different CAR T cells mediate different patterns and severity of side effects. The fact these characteristics are different between studies suggest that CAR design and manufacture play a role. Since CAR T cells behave differently in patients, it is likely that host factors also contribute.Further, whilst CD19 has been a successful target for CAR T cell therapy treating some forms of ALL and lymphoma, an important goal is to expand the indications for CAR T cell therapy to treat other blood cancers such as Acute Myeloid Leukaemia (AML). Finally, it is clear that targeting a single antigen can lead to tumours escaping recognition. As a result, we need to develop CAR T cells that target multiple antigens and understand the best CAR design for this.
The research aims of the group therefore are:
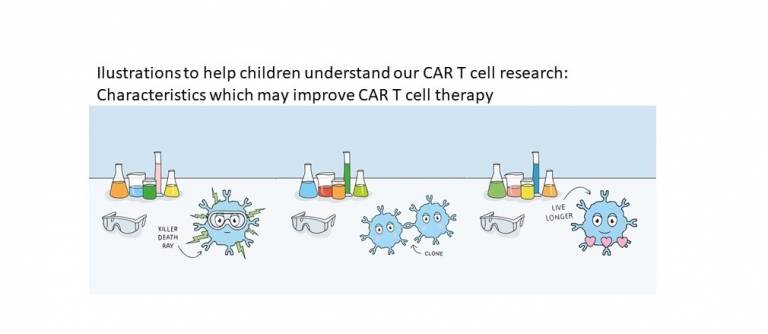
1) To investigate what makes a CAR T cell fit to mediate remission from cancer and persist long enough to cure the patient for good
2) To develop ways to improve the fitness and persistence of CAR T cells
3) To understand more about how CAR T cells recognise and are activated by cancer cells
4) To develop CAR T cell therapies for other haematological cancers, including Acute Myeloid Leukaemia (AML)
5) To work out what is the best CAR design when targeting multiple antigens
- Group Members
Mr Theo Accogli
Research Fellow
Email: theo.accogli@ucl.ac.uk
UCL Profiles page: Theo AccogliMr Jack Birch
Research Associate
Email: jack.birch@ucl.ac.ukMr Alex Puttick
PhD Student
Email: alexander.puttick.22@ucl.ac.uk
UCL Profiles page: Alexander Puttick- Funders

 Close
Close


