A summary of research published in the medical journal Lancet Digital Health prepared by the Multimorbidity Mechanism & Therapeutics Research Collaborative Patient and Public Involvement Group
Background
Study design
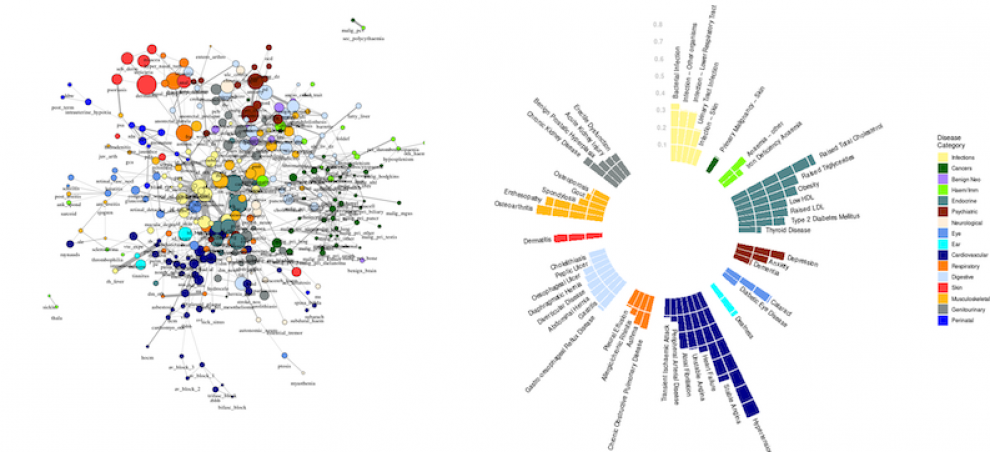
308 health conditions in nearly 4 million people were investigated. The team developed online interactive tools so that patterns of comorbidity and multimorbidity can be visualised.
Findings
The research team found many under-appreciated things. For instance, comorbidity and multimorbidity do not occur equally in men and women. More boys below 10 years of age had two or more diagnosed conditions than girls, but over the age of 10, the pattern reverses with more females diagnosed with multimorbidity. Researchers also found that more white individuals were diagnosed with multimorbidity compared to black or south Asian individuals.
This research found that depression co-occurs with a wide range of conditions: anxiety, obesity, atopy, migraine, deafness, soft tissue disorders, inflammatory disease and gastrointestinal conditions. Of these, national clinical guidelines for the treatment of depression published by NICE only mention anxiety and migraine.
Likewise, health research on a particular health condition often excludes people who also have other conditions. This means results may not reflect reality. For instance, heart failure often co-occurs with coronary heart disease, valvular disease, cardiac arrhythmias, lung diseases, musculoskeletal diseases, hypertension, renal insufficiency, type 2 diabetes and peripheral vascular disease, but people with these other conditions are often excluded from heart failure research.
Malignancy (cancer) and infection were most strongly linked to spinal fractures for black individuals but osteoporosis was the strongest link among white individuals. Associations between conditions also differ depending on age. For instance, hypertension was most strongly associated with kidney disorders in people aged 20-29 years but above 40 years the link with hypertension was strongest with dyslipidaemia (the imbalance of one or more kinds of lipid (fat) in your blood), obesity and diabetes.
How these findings will be used?
The results of this study have been published in the medical journal Lancet Digital Health. The open-access tools developed by the researchers provide a powerful resource for patients, policymakers and the clinical and pharmaceutical community to explore previously overlooked patterns in comorbidity and multimorbidity. The tools also have the potential to provide valuable insights into the detection, prevention and treatment of multimorbid health conditions.
Definitions
Comorbidity: The existence of more than one disease or condition in the same person at the same time. Comorbidities are usually long-term, or chronic and they may or may not interact with each other.
Multimorbidity: The occurrence of two or more co-existing chronic conditions in a patient over their lifetime.
Health data: Health data used in this study are any information "related to physical and mental health conditions, reproductive outcomes, causes of death, and quality of life" for an individual or population that is recorded in electronic health records.
NHS (National Health Service): Publicly funded health care provided in England, Scotland, Wales and Northern Ireland but each country has different organisation of its health services.
NICE (National Institute for Health and Care Excellence): Non-governmental body which sets standards and guidelines for health and social care in the UK.
 Close
Close

