HIV doesn't drive the spread of drug-resistant tuberculosis
9 August 2016
While the human immunodeficiency virus (HIV) pandemic fuels tuberculosis (TB) outbreaks, it does not drive the development and transmission of multidrug-resistance in TB patients as previously suspected, according to an international study led by UCL scientists.
The findings, published today in eLife, show that TB drug resistance is not more likely to evolve in HIV-positive patients compared to HIV-negative patients.
"We know that the HIV pandemic amplifies the TB epidemic as people are often co-infected but what wasn't clear before now was the effect of HIV on drug resistance of the agent of TB, the bacterium Mycobacterium tuberculosis (Mtb). We've shown for the first time that HIV is not the driver for multidrug-resistant TB," said co-first author Dr Adrien Rieux (UCL Genetics Institute).
"There are ongoing efforts around the world to tackle these potentially fatal diseases and it is know that among the estimated 1.5 million people who died from TB in 2015, about 200,000 cases involved multidrug-resistant TB and 400,000 were HIV co-infected." said co-first author Vegard Eldholm, a research fellow at the Norwegian Institute of Public Health.
To explore the impact of HIV co-infection on Mtb drug resistance, the team analysed the genomes of 252 TB isolates from patients belonging to the largest outbreak of multidrug-resistant TB in South America to date.
The isolates were collected from patients with known HIV status from the mid-1990s until 2009. The team used the genomes to create a time-labelled phylogenic tree, a diagram showing the inferred evolutionary relationships among the mutations within the sampled patients.
They then applied a new mathematical model optimised for TB to reconstruct how the disease spread among individuals. Finally, they combined the results of both methods to estimate the length of the TB latent period - the time from infection to infectiousness - and identify the patients in who TB strains evolved drug-resistance mutations.
"We saw no significant differences in the rate at which drug-resistant mutations occur in the genomes of strains in HIV-positive and negative patients. This suggests that drug resistance is not more likely to evolve in HIV-positive patients," said co-corresponding Francois Balloux, Professor of Computational Systems Biology (UCL Genetics Institute).
While the team's reconstruction of disease transmission among individuals did not reveal a significant impact of HIV co-infection on the ability of patients to transmit TB, their estimates of TB latency confirm that HIV co-infection accelerates the development of active TB.
"HIV prevents some cells from doing their job in the immune system, meaning the body is unable to fight off a large number of infections," Eldholm explained.
"The disease therefore provides TB with a pool of susceptible hosts, amplifying the rate of co-infection. Indeed, for this reason, HIV patients at a major hospital in Buenos Aires, Argentina, played a central role in fueling South America's largest multidrug-resistant TB epidemic in the early 1990s," Eldholm added.
Links
- Research paper in eLife
- Professor Francois Balloux's academic profile
- Dr Adrien Rieux's academic profile
- UCL Genetics Institute
- UCL Life Sciences
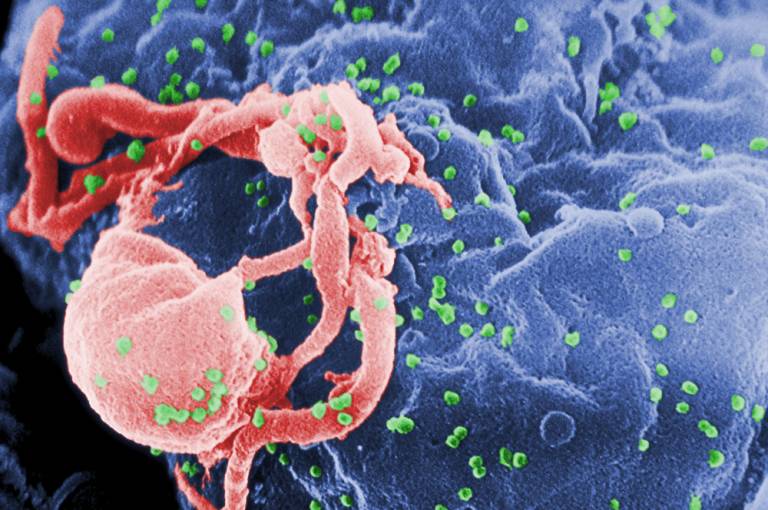
Image
- HIV budding (credit: C. Goldsmith, source: Wikimedia)
 Close
Close

