Bioengineering and Surgical Technology
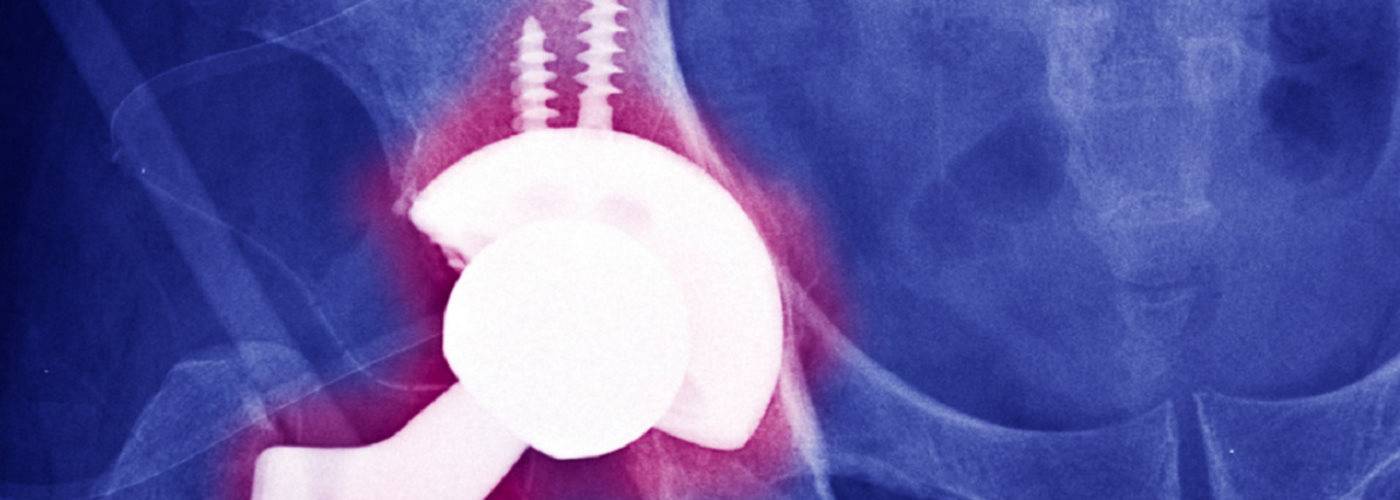
Making joint implants safer
Research by Professor Alister Hart has identified some causes of failed spine, hip, and knee implants. This has informed surgical decision-making and halted manufacture of unsafe implants.

Can marathon running improve knee damage?
A new study led by Professor Alister Hart has found that marathon running could improve knee damage in middle-aged adults who are new to running.
Our work
Musculoskeletal conditions are the most common cause of severe long-term pain and physical disability.
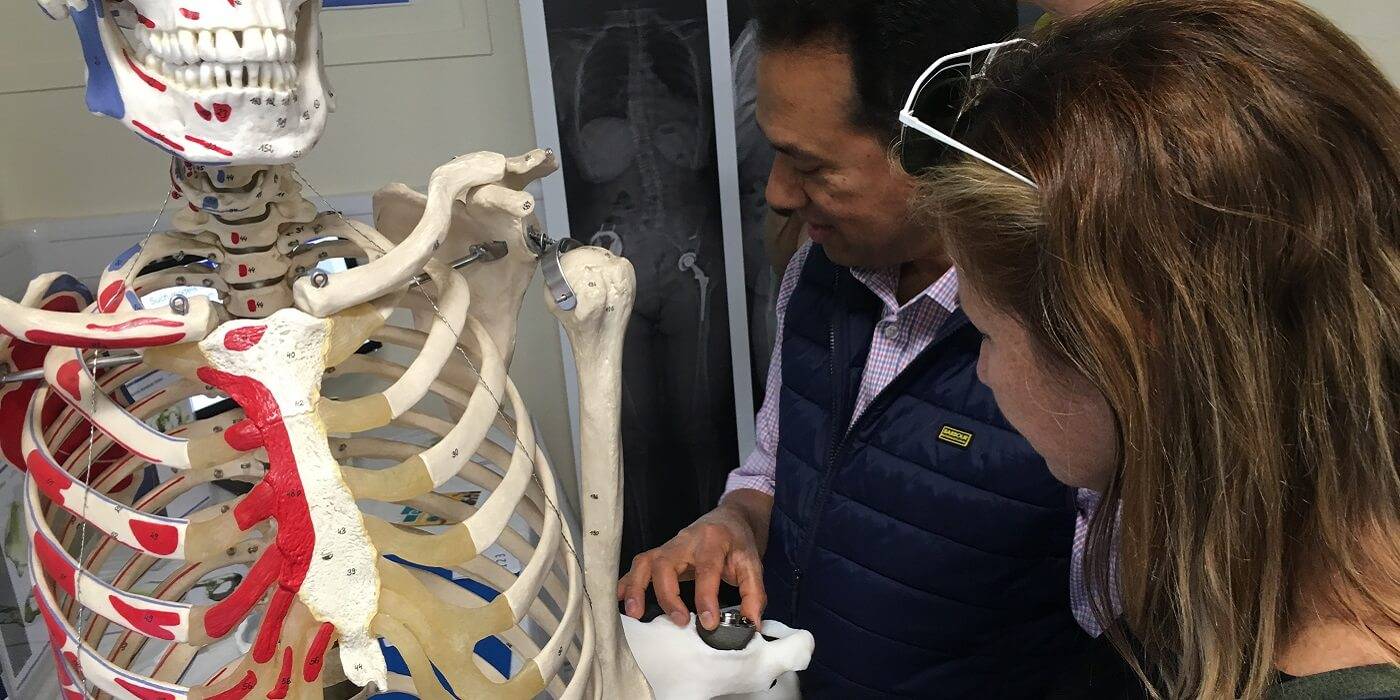
The success of musculoskeletal procedures relies on the development of materials combined with surgical techniques. Most joint replacements are used to replace worn out and damaged cartilage associated with osteoarthritis. Many other procedures involve the treatment of soft tissue injuries.
Our work increases the success of these procedures. We develop technology to replace, restore and regenerate musculoskeletal tissues through the interaction of innovative materials with surgical techniques, cells, and tissues.
What we do
Research: Translational stem cell research applied to scaffold materials used for the regeneration of musculoskeletal tissues. This involves an investigation of cell augmented scaffold and implants to enhance fixation to the bone and repair of tendons and ligaments.
Innovate surgical techniques associated with medical devices.
Develop innovative scaffolds, materials, and devices to regenerate, repair and replace the musculoskeletal system. These include the development of calcium phosphate bone graft substitutes, soft tissue scaffolds for tendon and ligament repair, and the use of new materials for osteochondral scaffolds.
Retrieve and analyse retrieved implants including joint replacements and spinal devices. We use retrieval data such as wear of implant articulating surfaces with patient details to assess implant success and predict performance. Our role informs surgeons and regulatory authorities about the failure of musculoskeletal devices.
Investigate new methods of reducing by killing or preventing biofilm formation on device surfaces. This work is associated with the development of bactericidal surfaces, anti-fouling implants and the use of new techniques to kill biofilms.
Our facilities


The Centre for Bioengineering and Surgical Technology

Head: Prof. Alister Hart





Select publications
- Buzasi, E., Kurakata, H., Gandhi, A., Birch, H.L., Zarnegar, R. & Best, L. (2022). The effects of booster sessions on self-management interventions for chronic musculoskeletal pain: a systematic review and meta-analysis of randomised controlled trials. Pain.
- Horga, L. M., Henckel, J., Fotiadou, A., Di Laura, A., Hirschmann, A. & Hart, A. (2021). 3.0 T MRI findings of 104 hips of asymptomatic adults: From non-runners to ultra-distance runners. BMJ Open Sport & Exercise Medicine, 7 (2), e000997.
- Ilo, K. C., Aboelmagd, K., Hothi, H. S., Asaad, A., Skinner, J. A. & Hart, A.J. (2021). Does modularity of metal-on-metal hip implants increase cobalt: chromium ratio? Hip International, ARTN 1120700019873637.
- Horga, L.M., Henckel, J., Fotiadou, A., Di Laura, A., Hirschmann, A. & Hart, A. (2021). Magnetic Resonance Imaging of the Hips of Runners Before and After Their First Marathon Run: Effect of Training for and Completing a Marathon. Orthopaedic Journal of Sports Medicine.
- Selim, O., Lakhani, S., Midha, S., Mosahebi, A. & Kalaskar, D.M. (2021). 3D Engineered Peripheral Nerve: Towards A New Era of Patient-Specific Nerve Repair Solutions. Tissue Eng Part B Rev.
- Eley, K. A., Moazen, M., Delso, G., Javidan, M., Kalaskar, D.M., et al. (2021). Enhancing Distraction Osteogenesis With Carbon Fiber Reinforced Polyether Ether Ketone Bone Pins and a Three-Dimensional Printed Transfer Device to Permit Artifact-Free Three-Dimensional Magnetic Resonance Imaging. Journal of Craniofacial Surgery.
- Yin, N.H., McCarthy, I. & Birch, H.L. (2021). An equine tendon model for studying intra-tendinous shear in tendons that have more than one muscle contribution. Acta Biomater.
- Farini, A., Sitzia, C., Villa, C., Cassani, B., Tripodi, L., Cerletti, M., et al. (2021). Defective dystrophic thymus determines degenerative changes in skeletal muscle. Nat Commun, 12 (1), 2099. doi:10.1038/s41467-021-22305-x
- Hale, L., Linley, E. & Kalaskar, D.M. (2020). A digital workflow for design and fabrication of bespoke orthoses using 3D scanning and 3D printing, a patient-based case study. Scientific Reports.
- Osagie-Clouard, L., Kaufmann, J., Blunn, G., Pendegrass, C., et al. (2019). Biomechanics of Two External Fixator Devices Used in Rat Femoral Fractures. Journal of Orthopaedic Research.
- Ulag, S., Ilhan, E., Sahin, A., Karademir Yilmaz, B., Kalaskar, D.M., Ekren, N., et al. (2020). 3D printed Artificial Cornea for Corneal Stromal Transplantation. European Polymer Journal, 109744.
- Burzyn, D., Wagers, A., Mathis, D. & Cerletti, M. (2019). Methods of Isolation and Analysis of TREG Immune Infiltrates from Injured and Dystrophic Skeletal Muscle. Methods Mol Biol, 1899, 229-237.
 Close
Close




