Feature: Why rare diseases are key for scientific discovery
28 February 2023
Rare diseases are varied and life-threatening, yet most still remain undiagnosed and have no effective treatments. Now, scientists at the UCL Neurogenetics Lab are focusing on these conditions, to find diagnoses and treatments that could be crucial for scientific discovery.
There is a common misconception that rare diseases only affect a small number of people. Yet there are currently 350 million patients who have a rare disease globally and around one in 17 people are affected by them at some point in their lives.
Scientists estimate there are more than 7,000 rare diseases in total – including Huntington’s disease, cystic fibrosis and muscular dystrophy. And they affect around 3.5 million people in the UK and 30 million across Europe.
Rare diseases are notoriously difficult to diagnose, and it can take years for patients to discover the cause of their symptoms.
This is partly because many conditions are so rare, it is challenging to obtain samples to rigorously study the diseases. Additionally, as 80% of rare diseases are caused by defective genes, previous technological limitations hindered researchers’ understanding of the genetic basis of these conditions.

Nevertheless, by applying the latest technologies in rare disease genetics research, scientists at the UCL Neurogenetics Lab at the UCL Queen Square Institute of Neurology hope their studies into rare and ultra-rare neurodevelopmental and neurological conditions will improve diagnosis and understanding of the underlying disease mechanisms.
Further, as many rare diseases are severe forms of more common diseases, studies on rare diseases are crucial for identifying cellular and molecular pathways that are associated with the development of other more common diseases, potentially impacting millions more people.
Here, the team highlight some of their astonishing findings:
Uncovering ancient gene mutation solves the mystery of neurological condition in people of European descent
Attributes Dr Reza Maroofian and colleagues

A seven-year-old girl came to Great Ormond Street Hospital as she struggled to climb the stairs and run. Despite performing extensive tests, doctors could not accurately diagnose her condition. Her mother was terrified by the idea that she may end up in a wheelchair; she wondered what they would say when she grew up, and how would they explain the disease to her.
Her parents also wondered how they could help her manage it, if they didn’t even know what it was.
When they would go on family walks, they would see the look of joy on their daughter’s face when she was riding a scooter but in the back of their minds there was the uncertainty about whether she would be able to do this in the future.
She was enrolled to the 100,000 Genomes project, in the hope that it would provide the family with some answers. Joining the project had an almost immediate impact on the family as a 7,000-year-old genetic mutation was identified in a gene called VWA1 that was hidden deep within her DNA.
After identifying this gene variant, we were able to identify several other families through the 100,000 Genomes Project database and other sequencing programmes who also had mutations in the same VWA1 gene. The other patients also had similar symptoms - a rare form of hereditary motor neuropathy.
On further investigation we also found that the primary mutation in VWA1 may be carried by one in 500 people of European descent.
Around one in a million are affected by the condition, which translates to more than 60 people in the UK alone - suggesting the condition may not be as rare as previously believed. At present, it is estimated that mutations in VWA1 may be responsible for up to 1% of unexplained neurological conditions in Europeans.
This demonstrates how widespread the impact of rare disease discoveries can be – as unlocking a single door could provide answers to a group of patients across an entire population.
Genetic testing & vitamin B6 supplementation led to patients’ regaining their ability to walk
Attributes Dr Viorica Chelban and colleagues

Two siblings in their seventies came to our clinic; for 30 years they had been suffering from an undiagnosed, progressive neurodegenerative disease. They were losing their vision and experienced increasing weakness in their arms and legs leaving them unable to perform many everyday tasks, with one of them becoming wheelchair bound.
Their concerns grew once they had families of their own about whether their children would also suffer from these debilitating symptoms. Since they were brother and sister there was a possibility that their condition resulted from an inherited genetic mutation, so we sequenced their DNA.
After long and careful analysis, we discovered they had a mutation in a gene that produces an enzyme called PDXK involved in the processing of vitamin B6.
We get B6 from our diet, but it needs to be activated by PDXK before it can be used in a host of biological functions – including the proper functioning of our peripheral nervous system. If the PDXK enzyme is absent or damaged, we cannot properly process and use the vitamin. When we checked the patients, we found that their levels of B6 were very low and knew we were onto something.
Having discovered the cause of the disease we set about working on potential treatments. Was there a way that we could bypass the faulty gene and give patients a modified form of vitamin B6 that their bodies could use?
We tried giving the patients a modified form of vitamin B6 via supplementation and remarkably, it worked better than we hoped. Within a few months of supplementation, the patients started recovering motor function, including one being able to leave his wheelchair and walk independently again.
When I first saw him walk, I was so surprised I kept asking him to walk up and down until eventually he said, “I’ll start running in a minute doctor.”
Publication of our discovery of the PDXK-related disease allowed clinicians and researchers from around the world to screen for mutations in this gene in patients with similar clinical problems.
Younger adults and children are now also being diagnosed and treated in the hope that they will never progress to the stage where they lose their sight and ability to walk.
This scenario highlights how combining the power of genetic testing with an understanding of the underlying cell biology can lead to life-changing treatments. The B6/PDXK story is one of those rare examples where we found the needle in the haystack – and were able to thread it.
An emotional journey from genetic discovery to creation of Rory Belle Foundation
Attributes Dr Stephanie Efthymiou and colleagues

When Rory Belle was born her parents had no idea that upon her birth, her body would begin to disintegrate - from her failure to grow, seizures and then liver failure. The list of symptoms increased at an endless pace that felt hard to comprehend. After whole exome sequencing was performed by a team in the US, mutations were discovered in a gene called NARS1.
The main challenge her parents struggled with was that the disease was so unknown, they were unsure of the best way to approach it. Their lack of understanding of the disorder unfortunately led to Rory Belle passing away without finding any resolution or even the name of the condition that took her life.
In the meantime, on the other side of the pond, researchers at UCL Queen Square Institute of Neurology and international collaborators studied a group of patients with different mutations in NARS1. Consequently, we helped to characterise the condition.
The quest to further understand the disease led to the creation of the Rory Belle Foundation, which our scientists helped to create and are now on the board of advisors for the foundation.
Rory Belle’s mother started the foundation in memory of her child to provide a community for other individuals in the world with symptoms related to NARS1 mutations.
From Rory Belle’s legacy that lives on through the foundation, many others born with NARS1 mutations live with the hope of one day having access to a gene replacement therapy.
Engaging families is essential for researchers to carry out their research; they play a pivotal role in supporting the research community in identifying other families with the same condition worldwide, enabling us to understand the underlying nature of the disease and aim to find safe and effective cures.
Unearthing a genetic mutation in a central Asian family ended the diagnostic odyssey in other parts of the world
Attributes Dr Rauan Kaiyrzhanov and colleagues

In many regions of the developing world there is limited or no access to genetic testing despite prevalence of undiagnosed or “difficult-to-diagnose” rare diseases being high.
A family came to our clinic in Kazakhstan, where all three children were affected with severe neurological disease where upon birth they had small heads, low height and weight and were later confirmed to be blind and deaf. Their condition progressively deteriorated leading to profound developmental delay. Alongside this, the mother suffered with the stigma that comes with giving birth to three children with neurodevelopmental conditions which weighed heavily on the parents’ relationship, leading to the father abandoning the family.
The mother was left alone and travelled all the way to India for medical tests on a quest to find a diagnosis for her children. Sadly she simply did not have the financial means for genetic testing, as it is expensive to perform.
However, in 2019 the family joined the UCL-Central Asia genomics project, where genetic testing was carried out as part of our research and eventually led to the identification of a mutation in a gene called SPATA5L.
After sharing our findings with other labs and colleagues around the world, we found over 27 affected individuals with similar conditions and different mutations in SPATA5L1. The effort not only made diagnosis possible for the family we were supporting but also helped the other families reach an accurate diagnosis for their children.
Following this, extensive experimental studies were performed to explore the disease-causing role of this gene and the mutations that were found in the families to further understand how these genes operate. At present, research is still in progress to understand the mechanisms of this disease, in the hope of developing future therapies.
This case highlights the importance of conducting genomic research in diverse populations and collaborating extensively - as the genomes of diverse individuals harbour a rich reservoir of information.
An unsolved conundrum from legendary neurologist solved 45 years later by new advanced genomic technologies
Attributes Dr Francesca Magrinelli and colleagues

A 45-year-old woman and her 15-year-old daughter presented to the Movement Disorders Centre at UCL with respiratory manifestations since birth, involuntary movements of their limbs (chorea) since infancy with gait impairment and sudden falls, thyroid dysfunction and abnormalities of the pituitary gland depicted on brain MRI.
The cause of this syndrome has remained a mystery since the time of Professor David Marsden, a pioneer and leader in the field of movement disorders who saw the mother at the National Hospital for Neurology and Neurosurgery at Queen Square, when she was a teenager. And all investigations failed to establish the cause of her symptoms.
However, by using a sophisticated bioinformatic analysis, our team were able to identify a long piece of “extra” DNA (Alu element) inserted out of place onto one copy of the gene NKX2-1, which is associated with brain-lung-thyroid syndrome. This Alu element first “jumped” inside the gene from another genomic region in the mother (her parents did not have this genetic defect) and was transmitted to her daughter, causing the protein product of this gene to be defective with consequences on the brain, thyroid, and lung.
This finding had not been possible even with the most comprehensive genetic tests available in the clinical setting. However, by extracting the Alu element from the patients’ DNA in the research genetics lab, we were able to include it in the DNA skeleton of bacteria to stretch it and make sequencing possible.
Huge collaborative efforts by young researchers in the UK and Germany provided this family with a genetic answer after a 45-year wait.
Advanced genomic technologies have enabled us to enter a new era in medical diagnosis, where technologies that were not previously available to us may allow many unsolved cases to finally reach a resolution and patients to get the answers they deserve.
Links
- UCL Neurogenetics Lab
- UCL Queen Square Institute of Neurology
- UCL Brain Sciences
- Dr Reza Maroofian's academic profile
- Dr Viorica Chelban's academic profile
- Dr Stephanie Efthymio's academic profile
- Dr Rauan Kaiyrzhano's academic profile
- Dr Francesca Magrinelli's academic profile
Image
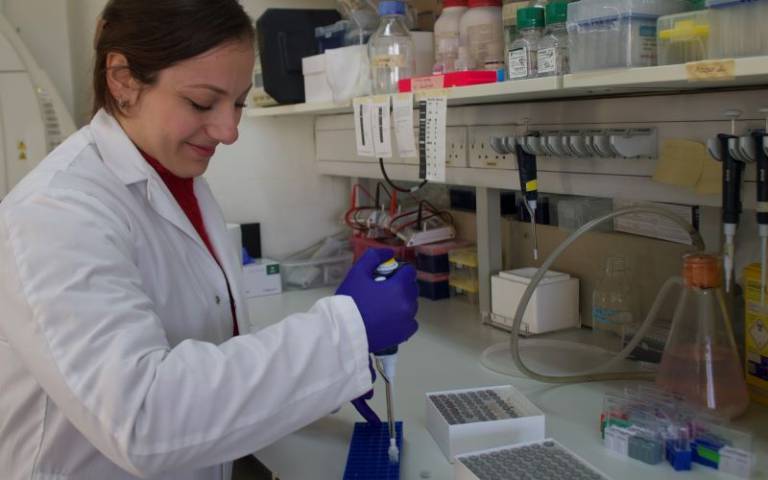
- UCL Neurogenetics Lab: Valentina Turchetti is preparing DNA samples extracted from the affected individuals for genetic testing.
- UCL Neurogenetics Lab: Annarita Scardamaglia is taking care of the cells taken from the patients for molecular and cell studies.
Media contact
Poppy Danby
E: p.danby [at] ucl.ac.uk
 Close
Close

