Genetic changes in tumours could predict patients' immunotherapy response
20 April 2021
Scientists at UCL, the Francis Crick Institute, and the Cancer Research UK Lung Cancer Centre of Excellence, have identified genetic changes in tumours which could be used to predict if immunotherapy drugs would be effective in individual patients.
Immunotherapies have led to huge progress treating certain types of cancer, but only a subset of patients respond, and hence a challenge for doctors and researchers is understanding why they work in some people and not others, and predicting who will respond well to treatment.
In their paper, published in Cell, the scientists looked for genetic and gene expression changes in tumours in over 1,000 patients being treated with checkpoint inhibitors, a type of immunotherapy which stops cancer cells from switching off the body’s immune response*.
They found that the total number of genetic mutations which are present in every cancer cell in a patient was the best predictor for tumour response to immunotherapy. The more mutations present in every tumour cell, the more likely they were to work. In addition, expression of gene CXCL9 was found to be a critical driver of an effective anti-tumour immune response.
The researchers also looked at the cases where checkpoint inhibitors had not been effective. For example, having more copies of a gene called CCND1 was linked to tumours being resistant to checkpoint inhibitors. More research is needed, but the scientists suggest that patients with this mutation in their tumours may benefit more from alternative drug treatment options.
Lead author, Dr Kevin Litchfield (UCL Cancer Institute), said: “This is the largest study of its kind, analysing genetic and gene expression data from across seven types of cancer and over a thousand people.
“It has enabled us to pinpoint the specific genetic factors which determine tumour response to immunotherapy, and combine them into a predictive test to identify which patients are most likely to benefit from therapy. Furthermore, it has improved our biological understanding of how immunotherapy works, which is vital for the design and development of new improved immunotherapeutic drugs.”
The researchers are now working with clinical partners in Denmark to see if their test correctly identifies the patients who will or will not respond to checkpoint inhibitors and if this is more accurate than tests currently available.
Corresponding author, Professor Charles Swanton (UCL Cancer Institute, the Crick, and chief clinician at Cancer Research UK), said: “Checkpoint inhibitors are really valuable in treating a number of cancers, including skin and lung cancers. But sadly, they do not always work and they can also sometimes cause severe side effects.
“If doctors have an accurate test, that tells them whether these drugs are likely to be effective in each individual patient, they will be able to make more informed treatment decisions. Crucially, they will be able to more quickly look for other options for patients who these drugs are unlikely to help.”
The work was partly funded by Cancer Research UK, the Royal Society, the Wellcome Trust, the Medical Research Council and Rosetrees Trust, among others.
* 1,008 patients treated with checkpoint inhibitors were included in the study. The seven tumour type groups are: metastatic urothelial cancer, malignant melanoma, head and neck cancer, non-small cell lung cancer, renal cell carcinoma, colorectal cancer and breast cancer.
Links
- Research paper published in Cell
- Professor Charles Swanton’s academic profile
- Dr Kevin Litchfield’s academic profile
- UCL Cancer Institute
- The Francis Crick Institute
- CRUK Lung Cancer Centre of Excellence
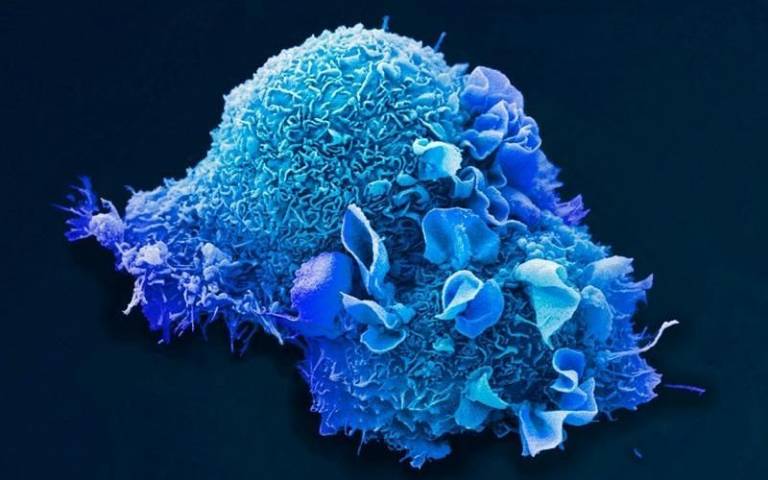
Image
- 'Lung cell', credit: Anne Weston. EM STP, The Francis Crick Institute
Media contact
Henry Killworth
Tel: +44 (0) 7881 833274
 Close
Close

