Prostate cancer screening using MRI for earlier diagnosis
5 April 2018
MRI scans could be used to detect prostate cancer more accurately, according to researchers at UCL, King's College London and Imperial College London who are launching a new clinical study.
The current prostate-specific antigen (PSA) blood test is considered too unreliable for population screening, and the researchers will test for the first time if MRI scans could be used to screen men to pick up cancers earlier and more reliably, and help save lives.
They will also study whether, combined with cutting-edge techniques such as genomics and machine learning, MRI scans can replace prostate biopsies.
"Our recent studies have begun to show how MRI technology will transform prostate cancer screening and diagnosis. Now we're starting an ambitious new study, to combine MRI with the latest technologies - such a machine learning on MRI images and detecting DNA shed by cancers in blood - to see if we can find a way to make prostate cancer testing more reliable and maybe even do away with the need for biopsies altogether," said lead researcher Professor Emberton (Dean, UCL Medical Sciences).
"We want to use MRI combined with new diagnostic tests to predict how the cancer will progress and to target the right treatment to the right person."
Prostate cancer patients advising the study say they are particularly excited by the prospect of large reduction in biopsies, as they have serious side effects in the majority of patients, which include pain, bleeding, infections leading to sepsis, and urine retention (sudden inability to empty the bladder).
The clinical study is being launched with funding of £4.1m from the Medical Research Council and £1m from Cancer Research UK, as part of the MRC's Stratified Medicine Initiative.
It builds on a ground-breaking study led by Professor Emberton and colleagues, published in The Lancet last year, which reported that MRI scans for men who had a positive PSA test could rule out prostate cancer in 27% of the men tested, meaning they could avoid having a biopsy. They also found that for men with a possible tumour, the MRI scan could be used to direct the biopsy needle to the right location, so 18% more cases of serious prostate cancer were detected.
The team aims to recruit 1,000 men with medium to high risk cancers, and hope to develop better diagnostic tests.
Professor Sir John Savill, until recently Chief Executive at the MRC, said: "Stratified medicine is reshaping the medical landscape by taking a patient-first approach that looks at how - and why - different groups of patients respond differently to therapies. Instead of looking for a 'one-size-fits-all' solution, stratified medicine is increasing what we know about diseases and how they affect individuals, and applying these findings to current tools in diagnostics and treatment to improve health outcomes."
Currently, the PSA blood test is considered unreliable because about 75% of men who get a positive result are not found to have cancer (a false positive), and it misses the cancer in about 15% of men with prostate cancer (a false negative).
In this study, the researchers will also be taking the MRI test out into the community for the first time to see how well it detects prostate abnormalities in 300 men aged 60 to 75 who have never had a PSA test.
Professor Emberton said: "We will be testing if the MRI can be used for screening men and we hope that it will detect serious cancers earlier that are currently missed. If we can detect cancers earlier and more reliably with a non-invasive test, this could help to improve the survival rates to prostate cancer, which kills about 11,800 men in the UK annually.
"MRI scanning for prostate cancer could also help a quarter of a million men, maybe up to half a million men a year, to avoid an unnecessary biopsy if the MRI is negative. The majority of men will be reassured they don't have prostate cancer and importantly they may be able to avoid the harms of a biopsy, plus healthcare systems will be able to avoid the costs. MRI is the perfect tool because it's relatively cheap, widely available and reliable."
Dr Ian Walker, Cancer Research UK's director of clinical research, said: "We're delighted to partner with the MRC to support such an ambitious project. Current tests are blunt and unreliable when it comes to helping doctors decide what course of action is best. Too many men are treated for cancers that would never have caused them harm and some cancers are missed altogether."
Links
- Professor Mark Emberton's academic profile
- UCL Medical Sciences
- Video interview with Prof Emberton
- 2017 Lancet paper
- Related UCL study: Prostate MRI scans increase cancer detection & reduce overdiagnosis
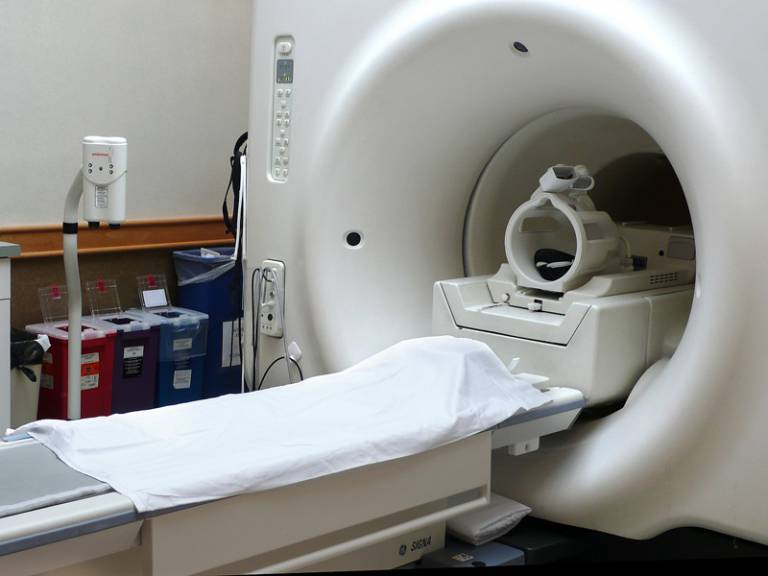
Image
- MRI scanner (Credit: Liz West, Source: Flickr)
Source
Media contact
Chris Lane
Tel: +44 (0)20 7679 9222
Email: chris.lane [at] ucl.ac.uk
 Close
Close

