Dr. Declan Chard
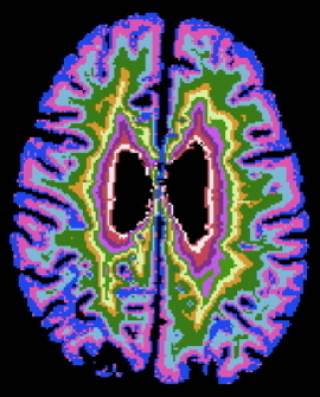
Multiple sclerosis (MS) has long been thought of as mainly a disease of brain white matter (WM), and its most obvious clinical feature (a relapse) is attributable to the formation of new WM lesions. However, in the longer term, many people with MS develop irreversible progressive disability unrelated to relapses, and it is thought that ultimately neurodegeneration is the main cause of this. We do not know what the principal driver of neurodegeneration is in MS.
In a series of related studies we are:
- Investigating mechanisms underlying neurodegeneration in MS - funded by the MRC.
- Identifying MRI features that can predict the development of progressive MS (and conversely features associated with clinical stability) - funded by the MS Society.
Developing new MRI measures for use in remyelination (in collaboration with colleagues in Cambridge) and progressive MS trials - funded by the MS Society, International Progressive MS Alliance (a collaborative project, led by colleagues in Montreal, Canada), and Hoffmann-La Roche.
 Close
Close