First ‘gene silencing’ drug for Alzheimer’s disease shows promise
25 April 2023
A world-first trial at UCL and UCLH has found a new genetic therapy for Alzheimer’s disease that is able to safely and successfully lower levels of the harmful tau protein known to cause the disease.
The trial, led by consultant neurologist Dr Catherine Mummery (UCL Queen Square Institute of Neurology & the National Hospital for Neurology and Neurosurgery), represents the first time that a ‘gene silencing’ approach has been taken in dementia and Alzheimer’s disease.
The approach uses a drug called BIIB080 (/IONIS-MAPTRx), which is an antisense oligonucleaotide (used to stop RNA producing a protein), to ‘silence’ the gene coding for the tau protein – known as the microtubule-associated protein tau (MAPT) gene. This prevents the gene from being translated into the protein in a doseable and reversible way. It will also lower the production of that protein and alter the course of disease.
Further trials will be needed in larger groups of patients to determine whether this leads to clinical benefit, but the phase 1 results published in Nature Medicine - with results from 46 patients - are the first indication that this method has a biological effect.
There are currently no treatments targeting tau. The drugs aducanumab and lecanemab – recently approved for use in some situations by the FDA – target a separate disease mechanism in AD, the accumulation of amyloid plaques*.
The phase 1 trial looked at the safety of BIIB080, what it does in the body, and how well it targets the MAPT gene. It involved the UCL Dementia Research Centre, was supported by the NIHR UCLH Biomedical Research Centre, was supported by the NIHR UCLH Biomedical Research Centre, and took place at the Leonard Wolfson Experimental Neurology Centre at NHNN.
46 patients, with an average age of 66, were enrolled in the trial – which took place from 2017 to 2020. The trial looked at three doses of the drug, given by intrathecal injection (an injection into the nervous system via the spinal canal), compared with the placebo.
Results show that the drug was well tolerated, with all patients completing the treatment period and over 90% completing the post-treatment period.
Patients in both the treatment and placebo groups experienced either mild or moderate side effects - the most common being a headache after injection of the drug. However, no serious adverse events were seen in patients given the drug.
The research team also looked at two forms of the tau protein in the central nervous system (CNS) – a reliable indicator of disease – over the duration of the study.
They found a greater than 50% reduction in levels of total tau and phosphor tau concentration in the CNS after 24 weeks in the two treatment groups that received the highest dose of the drug.
Dr Mummery said: “We will need further research to understand the extent to which the drug can slow progression of physical symptoms of disease and evaluate the drug in older and larger groups of people and in more diverse populations.
“But the results are a significant step forward in demonstrating that we can successfully target tau with a gene silencing drug to slow – or possibly even reverse – Alzheimer’s disease, and other diseases caused by tau accumulation in the future.”
Links
- Mummery, C.J., Börjesson-Hanson, A., Blackburn, D.J. et al. Tau-targeting antisense oligonucleotide MAPTRx in mild Alzheimer’s disease: a phase 1b, randomized, placebo-controlled trial. Nat Med (2023). https://doi.org/10.1038/s41591-023-02326-3
- Dr Cath Mummery’s academic profile
- Dementia Research Centre, UCL Queen Square Institute of Neurology
- UCLH
- National Hospital of Neurology & Neurosurgery
- *Lecanemab breakthrough
Image
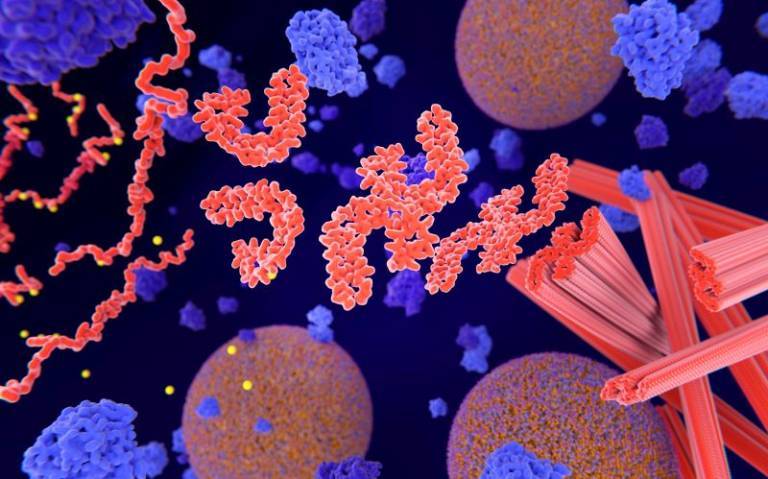
- Pathological phosphorylation (yellow) of Tau proteins (red-orange) leads to disintegration of microtubuli in the neuron axon an aggregation of the tau proteins. The transport of synaptic vesicles (orange-blue) is interrupted. Credit: selvanegra on iStock
 Close
Close

