New “chemical antibody” provides insight into origins of Parkinson’s disease
7 July 2022
Researchers have designed a new ‘chemical antibody’ that will help them understand the origins of neurological disorders such as Parkinson’s and Alzheimer’s disease.
In many neurodegenerative disorders, proteins become misfolded and form assemblies or ‘aggregates’ that are toxic to brain cells. It is now widely accepted that these larger aggregates are triggered by the accumulation of small, soluble protein bundles called oligomers. The larger, insoluble aggregates have been intensively studied using conventional methods. However, until now it has not been possible to accurately measure the concentrations of their rare precursor aggregates, or to determine their composition.
In a study published in Nature Chemistry, an international interdisciplinary team of researchers describe how they developed a new molecule that binds to these rare misfolded protein structures, thereby opening the way to a new understanding of how some of the world’s most devastating diseases originate.
The story starts with Professor Sonia Gandhi of the Francis Crick Institute and UCL Queen Square Institute of Neurology, who wanted to know how the smaller protein oligomer groups lead to the formation of larger aggregates and eventually to disease. “We have known that these structures are critical to detect,” she said, “But we have never been able to capture them, especially in patients.”
To solve this, Gandhi teamed up with physical and synthetic chemists, including Professors Sir David Klenerman and Steven Lee in the Yusuf Hamied Department of Chemistry, University of Cambridge, to design a new class of molecule that would target the oligomers.
“As physical chemists we understand how to design, modify and measure the processes of how small molecules interact with biological structures,” explained Klenerman. He and Lee worked together to design a molecule that would specifically bind to the protein aggregates. “We needed to be able to find a needle in a haystack,” said Lee.
The team conceived the idea of a ‘chemical antibody’, which unlike previously designed antibodies could be used to target the structure of protein aggregates rather than their linear sequence. The newly developed Y-shaped small molecule, dubbed “CAP-1” by the team, was designed to target the soluble protein oligomers and bind to them with high affinity, even in complex mixtures such as human cerebrospinal fluid. Lee explained: “Our new molecule uses the same design principles as found in nature – specifically antibodies – which have an amazing ability to stick to biological structures.”
Next Professor Tom Snaddon, an expert in chemical synthesis at Indiana University, helped design a way to make the new molecule in the laboratory. Professors Snaddon and Lee already had a long history of working together to create new molecules for tracking and understand neurodegenerative diseases. “The CAP-1 molecule poses very specific structural challenges” said Snaddon, “And it took many months of effort before the molecule could be successfully synthesized.”
Dr Margarida Rodrigues of the Faculty of Mathematics, University of Cambridge and first author of the paper, brought her biochemistry and biophysics background to help determine if the new molecule worked. “Developing a tool capable of isolating all small protein aggregates was exactly the type of exciting and challenging project that would take on,” said Rodrigues. “I was particularly motivated by the ‘out-of-the-box’ design of CAP-1 as compared to the traditional use of antibodies where you can only study one type of protein at a time.”
The researchers spent several years using advanced microscopy methods to investigate how CAP-1 works. They found the new chemical antibody is highly selective to the beta-sheet structure of the protein oligomers, and also has potential advantages in terms of stability and resistance to degradation compared to conventional antibodies. This means that these previously difficult-to-detect protein oligomers can be comprehensively investigated for the first time. ”It worked every time! It was so rewarding to ‘see’ CAP-1 capture the aggregates and recover them for further characterisation,” said Rodrigues.
The final step in the process was to find out if the molecule worked in human samples. The group collaborated with Professor Henrik Zetterberg of UCL Queen Square Institute of Neurology, the UK Dementia Research Institute and the University of Gothenburg, who has been studying biomarkers for Parkinson’s and Alzheimer’s diseases for over a decade.
A key experiment was to show that when CAP-1 was used in human cerebrospinal fluid from healthy individuals or patients with Parkinson’s, it could also detect protein aggregates in the fluid, and even enrich them for further studies.
“We anticipate these new tools and methods will be used to detect and characterise the aggregates that initiate and drive the development of neurodegenerative disorders such as Parkinson’s disease,” said Lee.
Links:
- Rodrigues et al. 'Structure-specific amyloid precipitation in biofluids' Nature Chemistry. Available online 7th July 2022. DOI: 10.1038/s41557-022-00976-3
- Professor Sonia Gandhi
- Professor Steven Lee
- TheLeeLab
- Professor Sir David Klenerman
- The Klenerman Lab
- Professor Tom Snaddon
- Professor Henrik Zetterberg
- Dr Margarida Dias Rodrigues
Source:
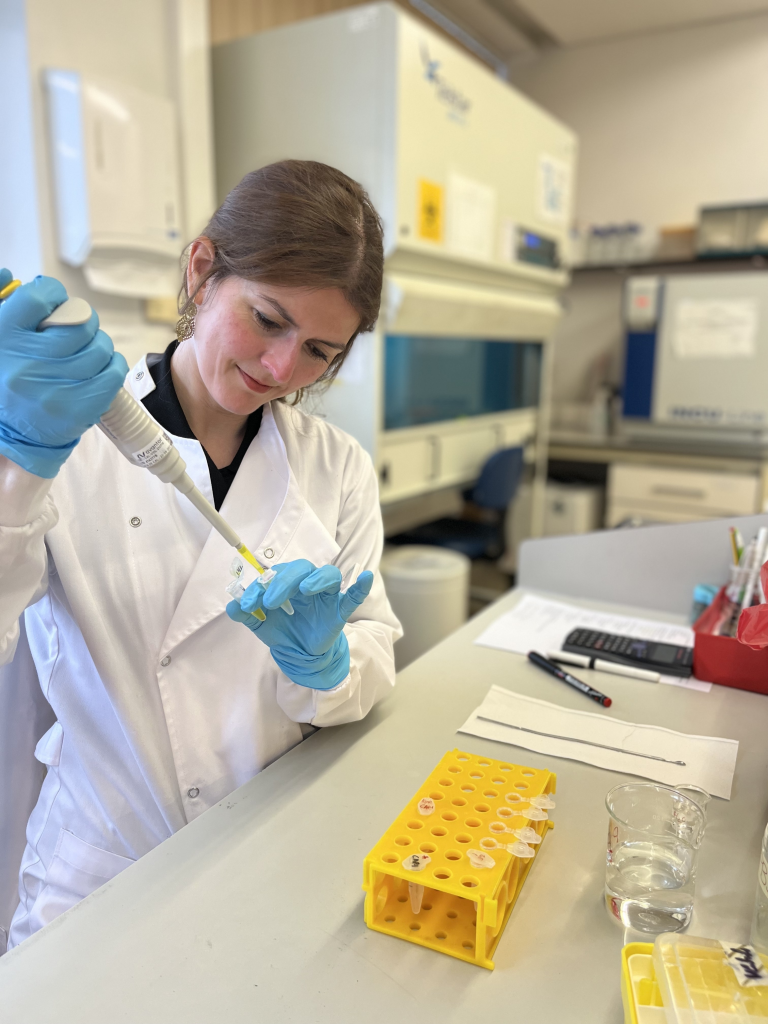
Image: Dr Margarida Dias Rodrigues working in the lab. Credir University of Cambridge.
 Close
Close

