Cerebral amyloid angiopathy (CAA) may be caused by prions
15 February 2019
A study published in Annals of Neurology, by Dr Gargi Banerjee and colleagues, led by Professor David Werring, UCL Queen Square Institute of Neurology, adds to evidence that prion diseases are more widespread and varied than had been realised
Three people who were diagnosed with cerebral amyloid angiopathy (CAA), a brain disease related to Alzheimer’s disease, likely developed the disease due to the transmission of amyloid pathology during neurosurgery decades earlier, according to the study. All three people had received cadaveric dura mater grafts – transplants of the tissue that covers the brain – when they were young, before developing CAA three to four decades later. The procedure was discontinued in the UK in 1992.
It’s the first case study of people who have received a CAA diagnosis during their lifetime attributed to neurosurgery, building on previous post-mortem evidence of possible amyloid transmission from dura mater grafts, contaminated neurosurgical instruments and growth hormone transplants.
CAA is a buildup of amyloid proteins that can cause strokes or brain bleeds, and typically occurs only in much older patients than the three people described in the study. CAA is often seen in people with Alzheimer’s disease, which is caused by the same buildup of proteins, but the patients in this study have not been diagnosed with Alzheimer’s. The three patients described in the study were in their 30s and 40s when they experienced symptoms including seizures, headaches and brain bleeds, and were diagnosed with CAA.
They were the only patients out of 663 referred to a specialist intracerebral haemorrhage service (the cases reviewed in the study) who had been diagnosed with CAA before age 50. All three patients had received dura mater grafts three to four decades earlier.
The researchers say that doctors need to be aware of the risk of amyloid transmission contributing to CAA. In patients over 55, CAA can occur sporadically, but would normally not be considered as a diagnosis in younger patients – but this study adds to evidence that, particularly with younger patients presenting with CAA-related symptoms, doctors should ask if they have had neurosurgery earlier in life.
While there is no cure for CAA, there are ways to reduce the associated risks of stroke and brain bleeds if doctors have the right diagnosis, as they can avoid blood thinners and closely monitor the patient’s blood pressure.
Further information:
- Banerjee et al. (2019) Early onset cerebral amyloid angiopathy following childhood exposure to cadaveric dura. Annals of Neurology 2019;85:284-90.
- Professor Werring's academic profile
- Dr Banerjee's academic profile
- Economist article
- Amyloid protein transmission through neurosurgery
- Amyloid pathology transmission in lab mice and historic medical treatments
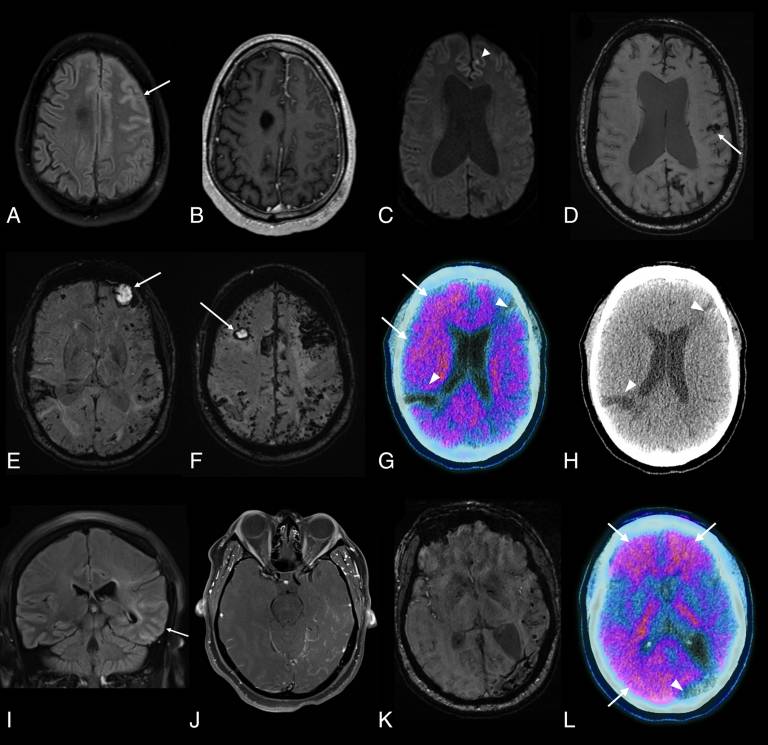
Image:
Brain Image Findings Banerjee et al. (2019)
 Close
Close

